Mild Electric Current Disrupts Bacterial Biofilms
|
By HospiMedica International staff writers Posted on 15 Dec 2016 |

Image: An example of biofilm formation (Photo courtesy of WSU).
A novel wound-healing technology uses an electrochemical scaffold (e-scaffold) and enhanced antibiotic susceptibility to eradicate biofilms and persister cells.
Researchers at Washington State University (Spokane, WA, USA) used an e-scaffold made out of conductive carbon fabric and a mild electrical current to produce a low, constant concentration of hydrogen peroxide (H2O2, an effective disinfectant) at the e-scaffold surface. The H2O2 disrupts the biofilm matrix and damages the bacteria cell walls and DNA, which allows better antibiotic penetration and efficacy against subpopulations of persister cells that survive treatment and are able to grow and multiply, resulting in chronic infections.
The researchers found that the e-scaffold enhanced tobramycin susceptibility in P. aeruginosa biofilms, which reached a maximum susceptibility at 40 µg/ml tobramycin, leading to complete elimination. In addition, the e-scaffold eradicated persister cells in the biofilms, leaving no viable cells. The researchers also observed that the e-scaffold induced intracellular formation of hydroxyl free radicals and improved membrane permeability in biofilm cells, which possibly enhanced the antibiotic susceptibility and eradication of persister cells. The study was published on November 23, 2016, in npj Biofilms and Microbiomes.
“Similar to the way that penicillin was discovered by accident, the research to develop the e-scaffold actually came out of a failed attempt to improve fuel cells,” said lead author Professor Haluk Beyenal, PhD, of the WSU School of Chemical Engineering and Bioengineering. “As engineers, we are always trying to find solutions to a problem, so we decided to use bad cathodes to control biofilm growth, and it worked. Our inspiration came from the fundamental work to understand its mechanism.”
Biofilms protect bacterial communities in part because the extracellular polymeric substances (EPS) that form the biofilm matrix serve as a diffusion barrier that limits antibiotic penetration and immobilizes antibiotics. The diffusive barrier also results in nutrient gradients, causing decreased growth and metabolic inactivity in parts of the biofilm community, which allows persister cells to arise. Increased persister cell formation is particularly observed in Gram-negative bacterial biofilms, as their cell membranes are composed of lipopolysaccharides that further limit antibiotic penetration.
Related Links:
Washington State University
Researchers at Washington State University (Spokane, WA, USA) used an e-scaffold made out of conductive carbon fabric and a mild electrical current to produce a low, constant concentration of hydrogen peroxide (H2O2, an effective disinfectant) at the e-scaffold surface. The H2O2 disrupts the biofilm matrix and damages the bacteria cell walls and DNA, which allows better antibiotic penetration and efficacy against subpopulations of persister cells that survive treatment and are able to grow and multiply, resulting in chronic infections.
The researchers found that the e-scaffold enhanced tobramycin susceptibility in P. aeruginosa biofilms, which reached a maximum susceptibility at 40 µg/ml tobramycin, leading to complete elimination. In addition, the e-scaffold eradicated persister cells in the biofilms, leaving no viable cells. The researchers also observed that the e-scaffold induced intracellular formation of hydroxyl free radicals and improved membrane permeability in biofilm cells, which possibly enhanced the antibiotic susceptibility and eradication of persister cells. The study was published on November 23, 2016, in npj Biofilms and Microbiomes.
“Similar to the way that penicillin was discovered by accident, the research to develop the e-scaffold actually came out of a failed attempt to improve fuel cells,” said lead author Professor Haluk Beyenal, PhD, of the WSU School of Chemical Engineering and Bioengineering. “As engineers, we are always trying to find solutions to a problem, so we decided to use bad cathodes to control biofilm growth, and it worked. Our inspiration came from the fundamental work to understand its mechanism.”
Biofilms protect bacterial communities in part because the extracellular polymeric substances (EPS) that form the biofilm matrix serve as a diffusion barrier that limits antibiotic penetration and immobilizes antibiotics. The diffusive barrier also results in nutrient gradients, causing decreased growth and metabolic inactivity in parts of the biofilm community, which allows persister cells to arise. Increased persister cell formation is particularly observed in Gram-negative bacterial biofilms, as their cell membranes are composed of lipopolysaccharides that further limit antibiotic penetration.
Related Links:
Washington State University
Latest Critical Care News
- Novel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
- Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
- Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
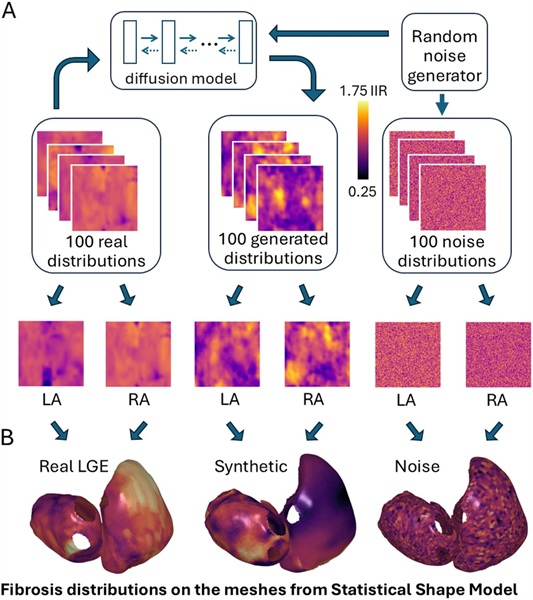
- Generative AI Technology Detects Heart Disease Earlier Than Conventional Methods
- Wearable Technology Predicts Cardiovascular Risk by Continuously Monitoring Heart Rate Recovery
- Wearable Health Monitoring Device Measures Gases Emitted from and Absorbed by Skin
- Groundbreaking Technology Rapidly Detects Airborne Influenza Viruses
- Handheld Device Could Transform Heart Disease Screening
- Flexible Semi-Autonomous Robot Could Deliver Medicine Inside Body

- Neurorestorative Treatment Strategies Hold Promise for Most Severe Forms of Epilepsy
- Gene Discovery Could Help Grow New Heart Arteries
- Study Discovers Invisible Transmission of Common Hospital-Associated Infection
- Non-Invasive Neuro-Ophthalmology Techniques Could Detect Brain Tumors Earlier
- Mass Manufactured Nanoparticles to Deliver Cancer Drugs Directly to Tumors
- World’s Smallest Pacemaker Fits Inside Syringe Tip

- AI-Powered, Internet-Connected Medical Devices to Revolutionize Healthcare, Finds Study
Channels
Surgical Techniques
view channel
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more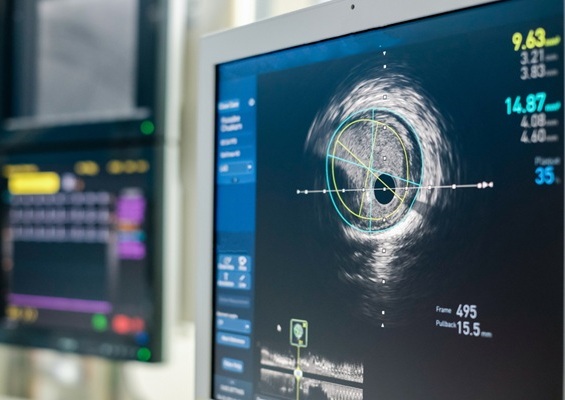
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more