Polypharmacy Associated with Frailty in Older People
|
By HospiMedica International staff writers Posted on 16 Feb 2017 |
A new study reveals that people taking more than 10 medicines are twice as likely to become frail within three years as people who take less than five.
Researchers at the German Cancer Research Center, the University of Heidelberg, and other institutions conducted a longitudinal, observational cohort study involving 3,058 community-dwelling adults aged 57 to 84 years in Saarland (Germany) to investigate the relationship between polypharmacy and frailty. Polypharmacy and hyper-polypharmacy were defined as the concomitant use of five or more and 10 or more drugs, respectively.
The results revealed that people who were at risk for frailty, as well as those who were already frail, were more likely to be in the polypharmacy or hyper-polypharmacy groups compared with people who were not. The researchers also concluded that those who took 5-9 medicines were 1.5 times more likely to become frail within three years, when compared with people who took fewer than 5 medications, while those who took more than 10 medicines were twice as likely to become frail within the same time period. The study was published on December 26, 2016, in the Journal of the American Geriatrics Society.
“Further research should address the potential benefit of reducing of inappropriate polypharmacy and better pharmacotherapeutic management for preventing medication-associated frailty,” said lead author Kai-Uwe Saum, PhD, MPH, of DFKZ. “In a perfect world, your physician would talk about your medications with a pharmacist and a geriatrician. This might help to reduce avoidable multiple drug prescriptions and possibly also lessen medication-induced risks for frailty and other negative effects of unnecessary, avoidable polypharmacy.”
Frailty is theoretically defined as a clinically recognizable state of increased vulnerability resulting from aging-associated decline in reserve and function across multiple physiologic systems, such that the ability to cope with everyday or acute stressors is comprised. In the absence of a gold standard, frailty has been operationally defined as meeting three out of five phenotypic criteria: low grip strength, low energy, slowed waking speed, low physical activity, and/or unintentional weight loss.
Researchers at the German Cancer Research Center, the University of Heidelberg, and other institutions conducted a longitudinal, observational cohort study involving 3,058 community-dwelling adults aged 57 to 84 years in Saarland (Germany) to investigate the relationship between polypharmacy and frailty. Polypharmacy and hyper-polypharmacy were defined as the concomitant use of five or more and 10 or more drugs, respectively.
The results revealed that people who were at risk for frailty, as well as those who were already frail, were more likely to be in the polypharmacy or hyper-polypharmacy groups compared with people who were not. The researchers also concluded that those who took 5-9 medicines were 1.5 times more likely to become frail within three years, when compared with people who took fewer than 5 medications, while those who took more than 10 medicines were twice as likely to become frail within the same time period. The study was published on December 26, 2016, in the Journal of the American Geriatrics Society.
“Further research should address the potential benefit of reducing of inappropriate polypharmacy and better pharmacotherapeutic management for preventing medication-associated frailty,” said lead author Kai-Uwe Saum, PhD, MPH, of DFKZ. “In a perfect world, your physician would talk about your medications with a pharmacist and a geriatrician. This might help to reduce avoidable multiple drug prescriptions and possibly also lessen medication-induced risks for frailty and other negative effects of unnecessary, avoidable polypharmacy.”
Frailty is theoretically defined as a clinically recognizable state of increased vulnerability resulting from aging-associated decline in reserve and function across multiple physiologic systems, such that the ability to cope with everyday or acute stressors is comprised. In the absence of a gold standard, frailty has been operationally defined as meeting three out of five phenotypic criteria: low grip strength, low energy, slowed waking speed, low physical activity, and/or unintentional weight loss.
Latest Critical Care News
- AI Eye Scans Could Help Identify Heart Disease and Stroke Risk
- Digital Heart Twin Improves Diagnosis and Treatment of Cardiac Arrhythmias
- First-Of-Its-Kind AI-Powered Probability Scoring System Assesses Heart Failure with Preserved Ejection Fraction
- AI-Assisted Colonoscopy Detects More Polyps but Has Modest Effect on Cancer Risk
- Wearables Could Reduce Need for Continuous Blood Thinners in Patients with Atrial Fibrillation
- AI Model Provides Real-Time Sepsis Risk Alerts for Improving ICU Patient Survival
- AI Algorithm Improves Intravenous Nutrition for Premature Babies
- Smart Mirror Generates AI-Powered Health Insights by Analyzing Facial Blood Flow
- Painless Diabetes Patch to Replace Needle Pricks

- Sensory T-Shirt Monitors Patient’s Vitals After Urological Surgery for Cancer
- Super-Sensitive Radar Technology Warns of Serious Heart Issues
- Thermal Imaging Could Accurately Track Vital Signs for Early Disease Detection
- New Microfluidic Device Improves Safety of Leukemia Treatment for Children
- Precision Transfusion Approach Improves Outcomes in TBI Patients
- Predictive Model for Daily Risk Alerts in Sepsis Patients Enables Early Intervention
- Novel Technology Measures Intracranial Pressure More Accurately and Non-Invasively
Channels
Artificial Intelligence
view channel
Innovative Risk Score Predicts Heart Attack or Stroke in Kidney Transplant Candidates
Heart researchers have utilized an innovative risk assessment score to accurately predict whether patients being evaluated for kidney transplants are at risk for future major cardiac events, such as a... Read more
AI Algorithm Detects Early-Stage Metabolic-Associated Steatotic Liver Disease Using EHRs
Liver disease, which is treatable when detected early, often goes unnoticed until it reaches advanced stages. Metabolic-associated steatotic liver disease (MASLD), the most prevalent form of liver disease,... Read moreSurgical Techniques
view channel
New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
Aortic regurgitation is a condition in which the aortic valve does not close properly, allowing blood to flow backward into the left ventricle. This results in decreased blood flow from the heart to the... Read more
Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
The tricuspid valve is one of the four heart valves, responsible for regulating blood flow from the right atrium (the heart's upper-right chamber) to the right ventricle (the lower-right chamber).... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read morePoint of Care
view channel
Handheld, Sound-Based Diagnostic System Delivers Bedside Blood Test Results in An Hour
Patients who go to a doctor for a blood test often have to contend with a needle and syringe, followed by a long wait—sometimes hours or even days—for lab results. Scientists have been working hard to... Read more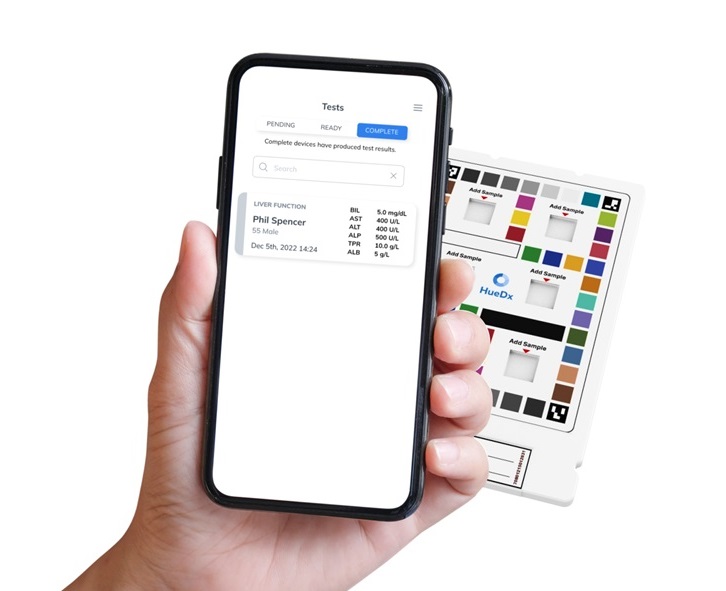
Smartphone-Enabled, Paper-Based Quantitative Diagnostic Platform Transforms POC Testing
Point-of-care diagnostics are crucial for public health, offering rapid, on-site testing that enables prompt diagnosis and treatment. This is especially valuable in remote or underserved regions where... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more