CLND Fails to Improve Melanoma Survival Rates
|
By HospiMedica International staff writers Posted on 19 Jun 2017 |
A new study shows that immediate completion lymph-node dissection (CLND) does not increase survival among patients with melanoma and sentinel-node metastases.
Researchers at the John Wayne Cancer Institute (JWCI; Santa Monica, CA, USA), Sentara CarePlex Hospital (Hampton, VA, USA), and other institutions worldwide conducted a study that randomly assigned 1,934 patients with sentinel-node metastases--detected via standard pathological assessment or a multimarker molecular assay--to immediate CLND or to an observation group monitored with ultrasonography. Main outcomes and measures were melanoma-specific survival, disease-free survival, and cumulative rate of non-sentinel-node metastasis.
The results showed that Immediate CLND was not associated with increased melanoma-specific survival. In the per-protocol analysis, the mean three-year rate of melanoma-specific survival was similar in the dissection group and the observation group (86%) at a median follow-up of 43 months. The mean rate of disease-free survival was slightly higher in the dissection group (68%) than in the observation group (63%) at three years. Lymphedema was observed in 24.1% of the patients in the dissection group and in 6.3% of those in the observation group. The study was published on June 8, 2017, in the New England Journal of Medicine (NEJM).
“Although the completion dissections did not help overall survival, they did have some value. By examining the dissected lymph nodes, physicians were able to better gauge how extensively the cancer had spread and to lengthen the time that their patients were disease-free. But those advantages did not translate into longer lives,” said lead author Mark Faries, MD, of JWCI. “The new findings likely will result in many fewer of these procedures being performed around the world. The results also will likely affect the design of many current and future clinical trials of medical therapies in melanoma.”
Lymph nodes, located throughout the body, serve as biologic filters that contain immune cells that fight infection and clean the blood. When cancer cells break away from a tumor, the cells can travel through the lymph system; sentinel node surgery allows the surgeon to remove the nodes to determine cancer spread. As human nodes are only 5 mm in size, they are difficult to discern from the surrounding tissue during surgery. Furthermore, even when surgeons are able to map the location of the nodes, there is no current technique that indicates whether or not the lymph nodes contain cancer, requiring removal of more lymph nodes than necessary.
Related Links:
John Wayne Cancer Institute
Sentara CarePlex Hospital
Researchers at the John Wayne Cancer Institute (JWCI; Santa Monica, CA, USA), Sentara CarePlex Hospital (Hampton, VA, USA), and other institutions worldwide conducted a study that randomly assigned 1,934 patients with sentinel-node metastases--detected via standard pathological assessment or a multimarker molecular assay--to immediate CLND or to an observation group monitored with ultrasonography. Main outcomes and measures were melanoma-specific survival, disease-free survival, and cumulative rate of non-sentinel-node metastasis.
The results showed that Immediate CLND was not associated with increased melanoma-specific survival. In the per-protocol analysis, the mean three-year rate of melanoma-specific survival was similar in the dissection group and the observation group (86%) at a median follow-up of 43 months. The mean rate of disease-free survival was slightly higher in the dissection group (68%) than in the observation group (63%) at three years. Lymphedema was observed in 24.1% of the patients in the dissection group and in 6.3% of those in the observation group. The study was published on June 8, 2017, in the New England Journal of Medicine (NEJM).
“Although the completion dissections did not help overall survival, they did have some value. By examining the dissected lymph nodes, physicians were able to better gauge how extensively the cancer had spread and to lengthen the time that their patients were disease-free. But those advantages did not translate into longer lives,” said lead author Mark Faries, MD, of JWCI. “The new findings likely will result in many fewer of these procedures being performed around the world. The results also will likely affect the design of many current and future clinical trials of medical therapies in melanoma.”
Lymph nodes, located throughout the body, serve as biologic filters that contain immune cells that fight infection and clean the blood. When cancer cells break away from a tumor, the cells can travel through the lymph system; sentinel node surgery allows the surgeon to remove the nodes to determine cancer spread. As human nodes are only 5 mm in size, they are difficult to discern from the surrounding tissue during surgery. Furthermore, even when surgeons are able to map the location of the nodes, there is no current technique that indicates whether or not the lymph nodes contain cancer, requiring removal of more lymph nodes than necessary.
Related Links:
John Wayne Cancer Institute
Sentara CarePlex Hospital
Latest Surgical Techniques News
- Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
- Novel Glue Prevents Complications After Breast Cancer Surgery
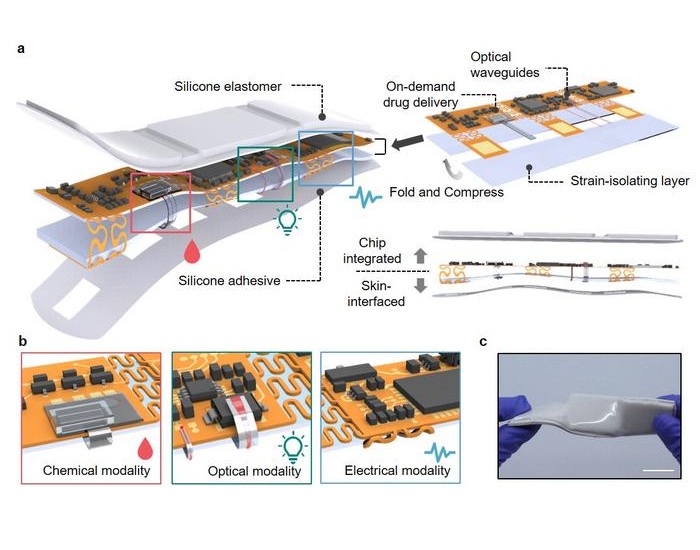
- Breakthrough Brain Implant Enables Safer and More Precise Drug Delivery
- Bioadhesive Sponge Stops Uncontrolled Internal Bleeding During Surgery
- Revolutionary Nano Bone Material to Accelerate Surgery and Healing
- Superior Orthopedic Implants Combat Infections and Quicken Healing After Surgery
- Laser-Based Technique Eliminates Pancreatic Tumors While Protecting Healthy Tissue
- Surgical Treatment of Severe Carotid Artery Stenosis Benefits Blood-Brain Barrier
- Revolutionary Reusable Duodenoscope Introduces 68-Minute Sterilization
- World's First Transcatheter Smart Implant Monitors and Treats Congestion in Heart Failure
- Hybrid Endoscope Marks Breakthrough in Surgical Visualization
- Robot-Assisted Bronchoscope Diagnoses Tiniest and Hardest to Reach Lung Tumors
- Diamond-Titanium Device Paves Way for Smart Implants that Warn of Disease Progression
- 3D Printable Bio-Active Glass Could Serve as Bone Replacement Material
- Spider-Inspired Magnetic Soft Robots to Perform Minimally Invasive GI Tract Procedures
- Micro Imaging Device Paired with Endoscope Spots Cancers at Earlier Stage
Channels
Critical Care
view channel
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read more
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more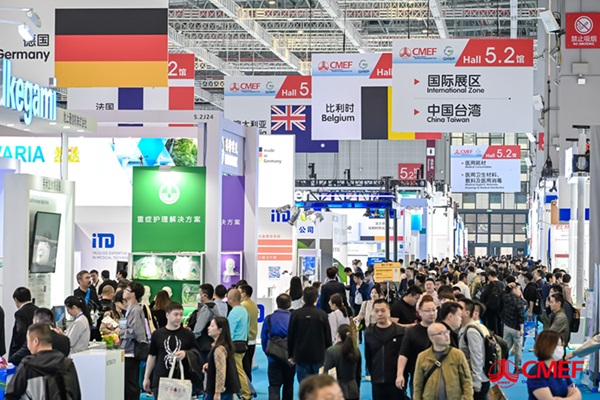
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more









.jpg)