Emergency Surgery Delays Linked to Higher Death Risk
|
By HospiMedica International staff writers Posted on 25 Jul 2017 |

Image: A new study claims delays in emergency surgery result in more deaths (Photo courtesy of Ottawa Hospital).
Delayed operating room access for emergency surgery increases mortality, lengthens hospital stay, and results in higher costs, claims a new study.
Researchers at Ottawa Hospital (Canada) and the University of Ottawa (Canada) conducted a study involving 15,160 patients who underwent emergency non-cardiac surgery between January 2012 and October 2014, in order to measure the impact of delay of emergency surgery on outcomes. Delay of surgery was defined as the time from surgical booking to operating room entry exceeding institutionally defined acceptable wait times, based on a standardized 5-level priority system that accounted for surgery type and indication.
The results revealed that 18.6% of patients experienced a delay, with mortality rates being 4.9% for those with delay, compared to 3.2% for those without delay, reflecting an odds ratio of 1.59. Delay was also significantly associated with increased length of stay and higher total costs. According to the researchers, the findings are consistent with evidence from other countries that delays are often due to system factors, and support the generalization of the delay-outcome association in orthopedic surgery. The study was published on July 10, 2017, in the Canadian Medical Association Journal (CMAJ).
“Delays in emergency surgeries are a problem around the world. This study adds to the evidence suggesting timely access to the operating room is important from both the patient and care provider perspectives,” concluded senior author Professor Alan Forster, MD, MSc, vice president of quality, performance, and population health at Ottawa Hospital. “To ensure emergency patients can be accommodated, it is necessary to have spare capacity. It might seem counterintuitive, but having unused time in expensive operating rooms could save both money and lives.”
“We found that most delays were due to system issues, like physician, nurse, and operating room unavailability. Improving personnel availability may improve access without increasing costs, at least from a hospital perspective,” said lead author Daniel McIsaac, MD, MPH, of Ottawa Hospital and the University of Ottawa. “Furthermore, the increased resources required to have adequate nursing personnel and physical resources should be partially offset by decreased hospital costs independently attributed to surgical delay.”
Related Links:
Ottawa Hospital
University of Ottawa
Researchers at Ottawa Hospital (Canada) and the University of Ottawa (Canada) conducted a study involving 15,160 patients who underwent emergency non-cardiac surgery between January 2012 and October 2014, in order to measure the impact of delay of emergency surgery on outcomes. Delay of surgery was defined as the time from surgical booking to operating room entry exceeding institutionally defined acceptable wait times, based on a standardized 5-level priority system that accounted for surgery type and indication.
The results revealed that 18.6% of patients experienced a delay, with mortality rates being 4.9% for those with delay, compared to 3.2% for those without delay, reflecting an odds ratio of 1.59. Delay was also significantly associated with increased length of stay and higher total costs. According to the researchers, the findings are consistent with evidence from other countries that delays are often due to system factors, and support the generalization of the delay-outcome association in orthopedic surgery. The study was published on July 10, 2017, in the Canadian Medical Association Journal (CMAJ).
“Delays in emergency surgeries are a problem around the world. This study adds to the evidence suggesting timely access to the operating room is important from both the patient and care provider perspectives,” concluded senior author Professor Alan Forster, MD, MSc, vice president of quality, performance, and population health at Ottawa Hospital. “To ensure emergency patients can be accommodated, it is necessary to have spare capacity. It might seem counterintuitive, but having unused time in expensive operating rooms could save both money and lives.”
“We found that most delays were due to system issues, like physician, nurse, and operating room unavailability. Improving personnel availability may improve access without increasing costs, at least from a hospital perspective,” said lead author Daniel McIsaac, MD, MPH, of Ottawa Hospital and the University of Ottawa. “Furthermore, the increased resources required to have adequate nursing personnel and physical resources should be partially offset by decreased hospital costs independently attributed to surgical delay.”
Related Links:
Ottawa Hospital
University of Ottawa
Latest Surgical Techniques News
- DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
- Tiny Robotic Tools Powered by Magnetic Fields to Enable Minimally Invasive Brain Surgery
- Magnetic Tweezers Make Robotic Surgery Safer and More Precise
- AI-Powered Surgical Planning Tool Improves Pre-Op Planning
- Novel Sensing System Restores Missing Sense of Touch in Minimally Invasive Surgery
- Headset-Based AR Navigation System Improves EVD Placement
- Higher Electrode Density Improves Epilepsy Surgery by Pinpointing Where Seizures Begin
- Open-Source Tool Optimizes Placement of Visual Brain Implants
- Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
Channels
Critical Care
view channel
AI Model Analyzes Patient Data to Diagnose Multiple Sclerosis With 90% Accuracy
Multiple sclerosis (MS) is a chronic inflammatory condition affecting the central nervous system. Most patients initially experience the relapsing-remitting form (RRMS), characterized by periods of symptom... Read more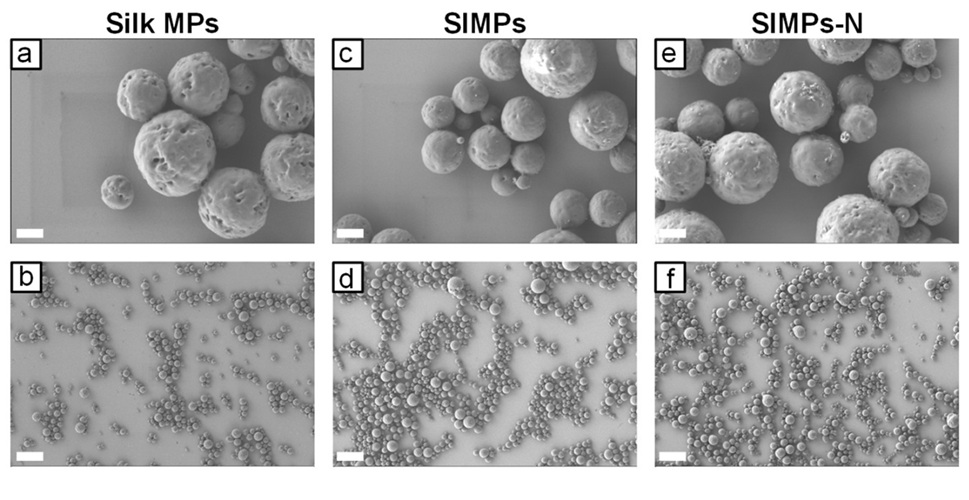
Magnetically Navigable Microparticles Enable Targeted Drug Delivery
Abdominal aortic aneurysms (AAA) can be life-threatening if not treated and result in nearly 10,000 deaths annually. Researchers working to improve treatments for AAA could now make it possible for doctors... Read more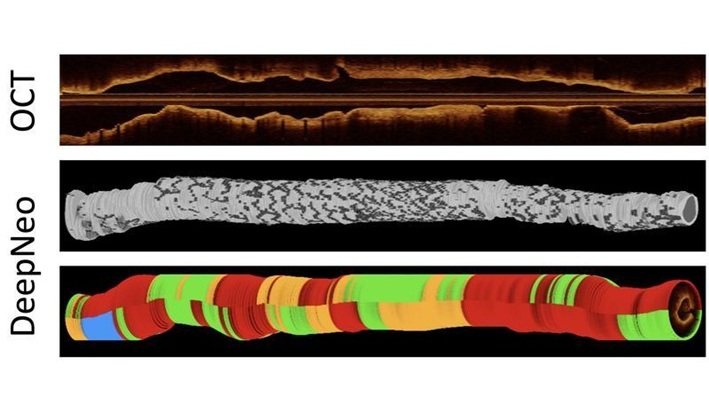
AI-Powered Algorithm Automates Analysis of Coronary Stents After Implantation
Every year, over three million people globally receive stents to open blocked blood vessels caused by heart disease. However, monitoring the healing process after stent implantation remains a significant challenge.... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more