TAVR Bleeding Complications Can Predict Mortality
|
By HospiMedica International staff writers Posted on 07 Aug 2017 |
Patients with severe aortic stenosis who experience bleeding complications following transcatheter aortic valve replacement (TAVR) face an increased risk for mortality, according to a new study.
Researchers at Swiss Cardiovascular Center Bern (CVRC; Switzerland) and the University of Bern (Switzerland) conducted a study involving 926 consecutive patients who underwent TAVR from 2007 through 2014 in order to examine frequency, timing, and association of access-site and non–access-site bleeding with mortality. Bleeding was assessed according to Valve Academic Research Consortium 2 (VARC2) criteria. The primary outcome of interest was all-cause mortality up to five years of follow-up.
The results revealed that 30.7% of patients had at least one subsequent bleeding event, which were split between bleeds from the access site and those at other sites. In all, 80% of the bleeding events occurred within the first 30 days after TAVR. In fact, all access-site bleeds took place during this early period; 40% of non-access-site bleeds happened later on throughout the follow-up period. For those who underwent transfemoral access, access-site bleeding did not significantly increase the risk of mortality, but non-access-site bleeding did.
Most access-site bleeds were minor, while non-access-site bleeds tended to be major. Minor bleeding was not significantly associated with mortality over follow-up, unlike major bleeds and life-threatening ones. Death from any cause was less likely for patients with access-site bleeds (58.7%) than non-access-site bleeds (72.8%). Analysis revealed that female sex was a significant correlate of access-site bleeding, whereas chronic kidney disease (CKD) was significantly associated with non–access-site bleeding. The study was published on July 24, 2017, in JACC: Cardiovascular Interventions.
“These findings parallel those observed in the field of percutaneous coronary intervention [PCI], in which non–access-related major bleeding complications have a significantly greater impact on mortality compared with access-site complications,” concluded senior author Stefan Stortecky, MD, of CVRC, and colleagues. “Non–access-site bleeding is a multifactorial event that encapsulates the patient risk profile as well as coexisting comorbidities, and whose risk is longitudinal and extends over time, which is not the case for access-site events that typically occur in the aftermath of the index procedure.”
The percutaneous treatment of severe aortic valve disease using prosthetic aortic valve replacement, without the need for open-heart surgery or cardiopulmonary bypass, is faster and less invasive than current open-heart procedures. TAVR has so far been proven effective in high-risk and inoperable patients, and could soon become the standard of care, even in moderate and low surgical risk patients.
Related Links:
Swiss Cardiovascular Center Bern
University of Bern
Researchers at Swiss Cardiovascular Center Bern (CVRC; Switzerland) and the University of Bern (Switzerland) conducted a study involving 926 consecutive patients who underwent TAVR from 2007 through 2014 in order to examine frequency, timing, and association of access-site and non–access-site bleeding with mortality. Bleeding was assessed according to Valve Academic Research Consortium 2 (VARC2) criteria. The primary outcome of interest was all-cause mortality up to five years of follow-up.
The results revealed that 30.7% of patients had at least one subsequent bleeding event, which were split between bleeds from the access site and those at other sites. In all, 80% of the bleeding events occurred within the first 30 days after TAVR. In fact, all access-site bleeds took place during this early period; 40% of non-access-site bleeds happened later on throughout the follow-up period. For those who underwent transfemoral access, access-site bleeding did not significantly increase the risk of mortality, but non-access-site bleeding did.
Most access-site bleeds were minor, while non-access-site bleeds tended to be major. Minor bleeding was not significantly associated with mortality over follow-up, unlike major bleeds and life-threatening ones. Death from any cause was less likely for patients with access-site bleeds (58.7%) than non-access-site bleeds (72.8%). Analysis revealed that female sex was a significant correlate of access-site bleeding, whereas chronic kidney disease (CKD) was significantly associated with non–access-site bleeding. The study was published on July 24, 2017, in JACC: Cardiovascular Interventions.
“These findings parallel those observed in the field of percutaneous coronary intervention [PCI], in which non–access-related major bleeding complications have a significantly greater impact on mortality compared with access-site complications,” concluded senior author Stefan Stortecky, MD, of CVRC, and colleagues. “Non–access-site bleeding is a multifactorial event that encapsulates the patient risk profile as well as coexisting comorbidities, and whose risk is longitudinal and extends over time, which is not the case for access-site events that typically occur in the aftermath of the index procedure.”
The percutaneous treatment of severe aortic valve disease using prosthetic aortic valve replacement, without the need for open-heart surgery or cardiopulmonary bypass, is faster and less invasive than current open-heart procedures. TAVR has so far been proven effective in high-risk and inoperable patients, and could soon become the standard of care, even in moderate and low surgical risk patients.
Related Links:
Swiss Cardiovascular Center Bern
University of Bern
Latest Surgical Techniques News
- DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
- Tiny Robotic Tools Powered by Magnetic Fields to Enable Minimally Invasive Brain Surgery
- Magnetic Tweezers Make Robotic Surgery Safer and More Precise
- AI-Powered Surgical Planning Tool Improves Pre-Op Planning
- Novel Sensing System Restores Missing Sense of Touch in Minimally Invasive Surgery
- Headset-Based AR Navigation System Improves EVD Placement
- Higher Electrode Density Improves Epilepsy Surgery by Pinpointing Where Seizures Begin
- Open-Source Tool Optimizes Placement of Visual Brain Implants
- Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
Channels
Critical Care
view channel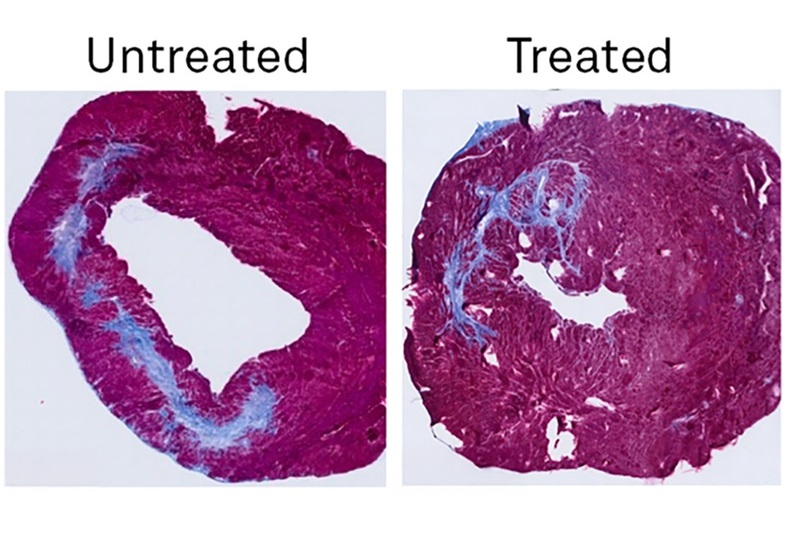
New Potent Injectable Therapy Could Prevent Heart Failure After Heart Attack
According to the U.S. Centers for Disease Control and Prevention, 6.7 million Americans aged 20 and older are living with heart failure, a condition in which the heart cannot pump enough blood to meet... Read more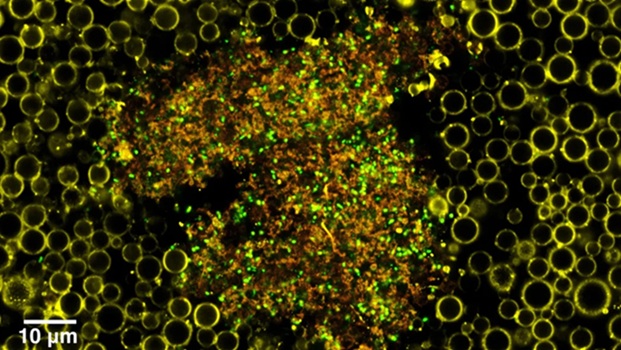
Drug Delivery System Uses Ultrasound-Activated Nanoparticles to Destroy Bacterial Biofilms
Chronic antibiotic-resistant infections have become a global health crisis, impacting hundreds of millions of individuals worldwide. In as many as 80% of chronic infections, bacteria form biofilms—slimy... Read more
Hospital-Based System Combines AI and Genomic Surveillance to Quickly Detect Infectious Disease Outbreaks
The current approach used by hospitals to detect and prevent the transmission of infectious diseases among patients is outdated. These methods have remained largely unchanged for over a century.... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more