Expedited Surgery Imperative for Post-Hip Fracture Survival
|
By HospiMedica International staff writers Posted on 20 Aug 2018 |
Surgery on admission day or the following day reduces postoperative mortality among medically stable patients with hip fracture, according to a new study.
Researchers at the University of British Columbia (UBC; Vancouver, Canada), the University of Toronto (UT; Canada), and other institutions analyzed data regarding 139,119 medically stable patients with first-time hip fracture (65 years or older, 74% female) who underwent surgery at 144 hospitals throughout Canada--excluding the province of Quebec--between 2004 and 2012. Expected population-average risks of inpatient death within 30 days were calculated for patients surgically treated on the day of admission, inpatient day two, day three, or after day three.
The results revealed that 23.1% underwent surgery on admission day, 43.5% underwent surgery on inpatient day two, 21% on day three, and 12.4% at a later date. Cumulative 30-day in-hospital mortality was 4.9% among patients who were surgically treated on admission day, increasing to 6.9% for surgery done after day three. The researchers projected an additional 10.9 deaths per 1,000 surgeries if all surgeries were done after inpatient day three instead of admission day. The study was published on August 7, 2018, in the Canadian Medical Association Journal (CMAJ).
“Our findings allow us to infer a critical point for the timing of hip fracture repair. We suggest that clinicians, administrators, and policy-makers 'not let the sun set twice' on medically stable older adults before their hip fracture repair,” said co-lead author orthopedic surgeon Pierre Guy, MD, of UBC. “We estimate that 16.5% of in-hospital deaths currently occurring in patients delayed for more than two days are avoidable by adopting the 'don't let the sun set twice' policy for hip fracture patients.”
Canadian hospitals admit 30,000 older adults with hip fracture annually. Such patients face an increased risk of death, with up to 5% of women and 10% of men dying within 30 days. Early surgical intervention improves survival by reducing patients’ exposure to immobilization and inflammation. In 2005, Canada established a benchmark of 48 hours from admission for 90% of hip fracture surgeries so as to prevent potentially harmful delays. But delays remain common, and many patients who are medically stable at presentation may have to wait until a surgeon or an operating room becomes available.
Related Links:
University of British Columbia
University of Toronto
Researchers at the University of British Columbia (UBC; Vancouver, Canada), the University of Toronto (UT; Canada), and other institutions analyzed data regarding 139,119 medically stable patients with first-time hip fracture (65 years or older, 74% female) who underwent surgery at 144 hospitals throughout Canada--excluding the province of Quebec--between 2004 and 2012. Expected population-average risks of inpatient death within 30 days were calculated for patients surgically treated on the day of admission, inpatient day two, day three, or after day three.
The results revealed that 23.1% underwent surgery on admission day, 43.5% underwent surgery on inpatient day two, 21% on day three, and 12.4% at a later date. Cumulative 30-day in-hospital mortality was 4.9% among patients who were surgically treated on admission day, increasing to 6.9% for surgery done after day three. The researchers projected an additional 10.9 deaths per 1,000 surgeries if all surgeries were done after inpatient day three instead of admission day. The study was published on August 7, 2018, in the Canadian Medical Association Journal (CMAJ).
“Our findings allow us to infer a critical point for the timing of hip fracture repair. We suggest that clinicians, administrators, and policy-makers 'not let the sun set twice' on medically stable older adults before their hip fracture repair,” said co-lead author orthopedic surgeon Pierre Guy, MD, of UBC. “We estimate that 16.5% of in-hospital deaths currently occurring in patients delayed for more than two days are avoidable by adopting the 'don't let the sun set twice' policy for hip fracture patients.”
Canadian hospitals admit 30,000 older adults with hip fracture annually. Such patients face an increased risk of death, with up to 5% of women and 10% of men dying within 30 days. Early surgical intervention improves survival by reducing patients’ exposure to immobilization and inflammation. In 2005, Canada established a benchmark of 48 hours from admission for 90% of hip fracture surgeries so as to prevent potentially harmful delays. But delays remain common, and many patients who are medically stable at presentation may have to wait until a surgeon or an operating room becomes available.
Related Links:
University of British Columbia
University of Toronto
Latest Surgical Techniques News
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
- Tiny Robotic Tools Powered by Magnetic Fields to Enable Minimally Invasive Brain Surgery
- Magnetic Tweezers Make Robotic Surgery Safer and More Precise
- AI-Powered Surgical Planning Tool Improves Pre-Op Planning
- Novel Sensing System Restores Missing Sense of Touch in Minimally Invasive Surgery
- Headset-Based AR Navigation System Improves EVD Placement
- Higher Electrode Density Improves Epilepsy Surgery by Pinpointing Where Seizures Begin
- Open-Source Tool Optimizes Placement of Visual Brain Implants
- Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
- Groundbreaking Leadless Pacemaker to Prevent Invasive Surgeries for Children
Channels
Critical Care
view channel
Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
Intestinal gases are associated with several health conditions, including colon cancer, irritable bowel syndrome, and inflammatory bowel disease, and they have the potential to serve as crucial biomarkers... Read moreNovel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
Multiphoton microscopy has become an invaluable tool in neuroscience, allowing researchers to observe brain activity in real time with high-resolution imaging. A crucial aspect of many multiphoton microscopy... Read more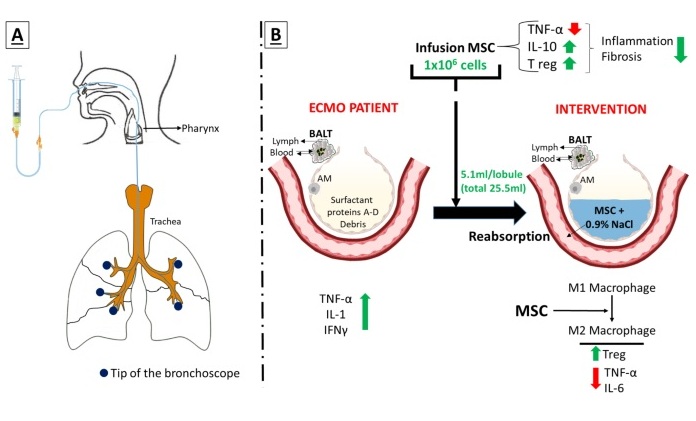
Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
Until now, administering cell therapies to patients on extracorporeal membrane oxygenation (ECMO)—a life-support system typically used for severe lung failure—has been nearly impossible.... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more