Sponge on a String Test Could Replace Endoscopies
|
By HospiMedica International staff writers Posted on 14 Aug 2020 |

The Cytosponge contained in the capsule and fully expanded (Photo courtesy of Cambridge University)
A minimally invasive sampling device to diagnose Barrett's esophagus (BE) can identify ten times more people than standard routes, claims a new study.
Developed by researchers at Cambridge University (United Kingdom), King’s College London (KCL; United Kingdom), and other institutions, the Cytosponge is made of a material with just enough abrasiveness to collect cells without damaging tissue. For the BE test, it is swallowed by the patient while still inside a dissolvable capsule with a string attached to it. Five minutes later, after the capsule has dissolved, the string is pulled to retrieve the sponge, collecting cells on the way. These are then sent to the lab for analysis, like a biopsy sample.
The test can be performed in a general practitioner’s (GP) office and can help doctors decide who needs to undergo a follow-up endoscopy. For the study, the researchers studied 13,222 participants who were randomly allocated to being offered the sponge test or regular care. Over the course of a year, the odds of detecting BE were tenfold in those offered the Cytosponge, with 140 cases diagnosed compared to 13 in usual care. In addition, the Cytosponge diagnosed five cases of early cancer, whereas only one case of early cancer was detected in the usual care group. The study was published on August 1, 2020, in The Lancet.
“It's taken almost a decade of research and testing thousands of patients to show that we've developed a better route to diagnosing Barrett's esophagus. And the sponge could also be a game-changer in how we diagnose and ensure more people survive esophageal cancer,” said lead author Professor Rebecca Fitzgerald, MD, of the University of Cambridge. “Compared with endoscopies performed in hospital, the Cytosponge causes minimal discomfort and is a quick, simple test that can be done by a GP. Our test is already being piloted around the country, so we hope more people across the UK could benefit from it.”
“The results of this trial exceeded my most optimistic expectations. Use of Professor Fitzgerald's simple invention will hopefully lead to a significant reduction in the number of people dying from esophageal cancer over the next 20 years,” said senior author Professor Peter Sasieni, PhD, of KCL. “This trial found that both patients and staff were happy with the Cytosponge test and it is practical to consider rolling it out within the NHS.”
Barrett's esophagus refers to an abnormal change (metaplasia) in the cells of the lower portion of the esophagus, when the normal squamous epithelium lining is replaced by goblet cells, which are usually found lower in the gastrointestinal tract. The medical significance of BE is its strong association with esophageal adenocarcinoma, a particularly lethal form of cancer.
Related Links:
Cambridge University
King's College London
Developed by researchers at Cambridge University (United Kingdom), King’s College London (KCL; United Kingdom), and other institutions, the Cytosponge is made of a material with just enough abrasiveness to collect cells without damaging tissue. For the BE test, it is swallowed by the patient while still inside a dissolvable capsule with a string attached to it. Five minutes later, after the capsule has dissolved, the string is pulled to retrieve the sponge, collecting cells on the way. These are then sent to the lab for analysis, like a biopsy sample.
The test can be performed in a general practitioner’s (GP) office and can help doctors decide who needs to undergo a follow-up endoscopy. For the study, the researchers studied 13,222 participants who were randomly allocated to being offered the sponge test or regular care. Over the course of a year, the odds of detecting BE were tenfold in those offered the Cytosponge, with 140 cases diagnosed compared to 13 in usual care. In addition, the Cytosponge diagnosed five cases of early cancer, whereas only one case of early cancer was detected in the usual care group. The study was published on August 1, 2020, in The Lancet.
“It's taken almost a decade of research and testing thousands of patients to show that we've developed a better route to diagnosing Barrett's esophagus. And the sponge could also be a game-changer in how we diagnose and ensure more people survive esophageal cancer,” said lead author Professor Rebecca Fitzgerald, MD, of the University of Cambridge. “Compared with endoscopies performed in hospital, the Cytosponge causes minimal discomfort and is a quick, simple test that can be done by a GP. Our test is already being piloted around the country, so we hope more people across the UK could benefit from it.”
“The results of this trial exceeded my most optimistic expectations. Use of Professor Fitzgerald's simple invention will hopefully lead to a significant reduction in the number of people dying from esophageal cancer over the next 20 years,” said senior author Professor Peter Sasieni, PhD, of KCL. “This trial found that both patients and staff were happy with the Cytosponge test and it is practical to consider rolling it out within the NHS.”
Barrett's esophagus refers to an abnormal change (metaplasia) in the cells of the lower portion of the esophagus, when the normal squamous epithelium lining is replaced by goblet cells, which are usually found lower in the gastrointestinal tract. The medical significance of BE is its strong association with esophageal adenocarcinoma, a particularly lethal form of cancer.
Related Links:
Cambridge University
King's College London
Latest Critical Care News
- Mechanosensing-Based Approach Offers Promising Strategy to Treat Cardiovascular Fibrosis
- AI Interpretability Tool for Photographed ECG Images Offers Pixel-Level Precision
- AI-ECG Tools Can Identify Heart Muscle Weakness in Women Before Pregnancy
- AI Model Analyzes Patient Data to Diagnose Multiple Sclerosis With 90% Accuracy
- Magnetically Navigable Microparticles Enable Targeted Drug Delivery
- AI-Powered Algorithm Automates Analysis of Coronary Stents After Implantation
- New Stroke Risk Scoring System to Help Avoid Unnecessary Surgeries
- Wearable Device Tracks Individual Cells in Bloodstream in Real Time
- Drug Delivery System Uses Ultrasound-Activated Nanoparticles to Destroy Bacterial Biofilms
- New Potent Injectable Therapy Could Prevent Heart Failure After Heart Attack
- Hospital-Based System Combines AI and Genomic Surveillance to Quickly Detect Infectious Disease Outbreaks
- New Approach to Visualizing Blood Pressure Data Can Help Better Manage Hypertension Patients
- Breakthrough AI Technology Accurately Assesses Heart Failure Severity
- Smart Bandage Monitors Chronic Wounds in Human Patients
- AI Identifies Patients with Increased Lung Cancer Risk Up To 4 Months Earlier
- Next Gen Hemodynamic Monitoring Solution Provides AI-Driven Clinical Decision Support
Channels
Surgical Techniques
view channel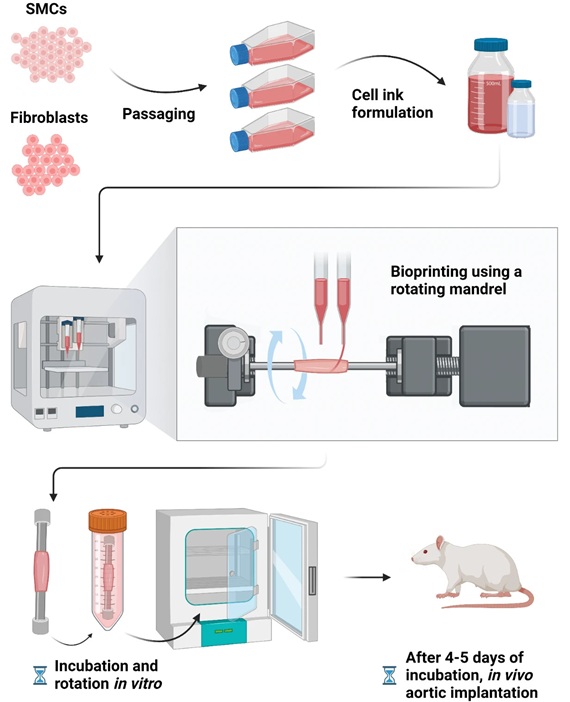
Bioprinted Aortas Offer New Hope for Vascular Repair
Current treatment options for severe cardiovascular diseases include using grafts made from a patient's own tissue (autologous) or synthetic materials. However, autologous grafts require invasive surgery... Read more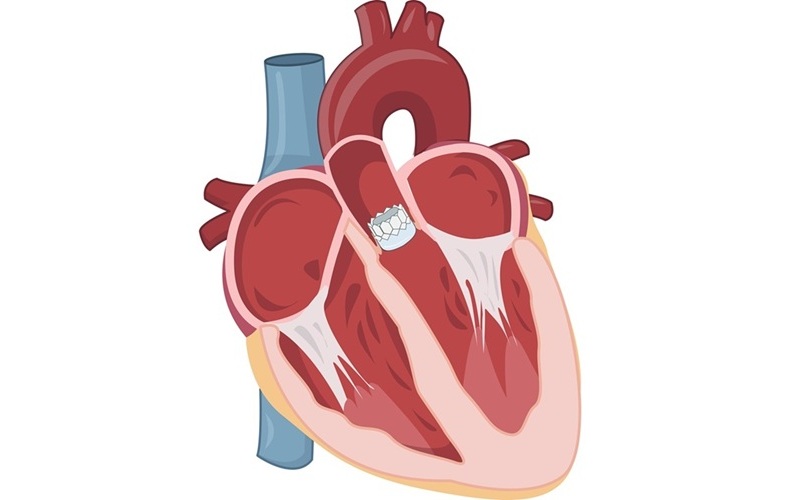
Early TAVR Intervention Reduces Cardiovascular Events in Asymptomatic Aortic Stenosis Patients
Each year, approximately 300,000 Americans are diagnosed with aortic stenosis (AS), a serious condition that results from the narrowing or blockage of the aortic valve in the heart. Two common treatments... Read more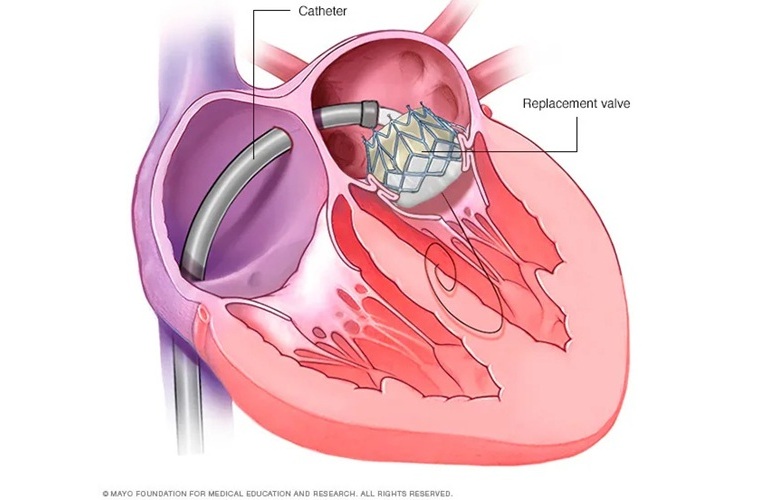
New Procedure Found Safe and Effective for Patients Undergoing Transcatheter Mitral Valve Replacement
In the United States, approximately four million people suffer from mitral valve regurgitation, the most common type of heart valve disease. As an alternative to open-heart surgery, transcatheter mitral... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more
















