Bio-Engineered Implant Helps Heal Torn ACLs 
|
By HospiMedica International staff writers Posted on 11 Jan 2021 |
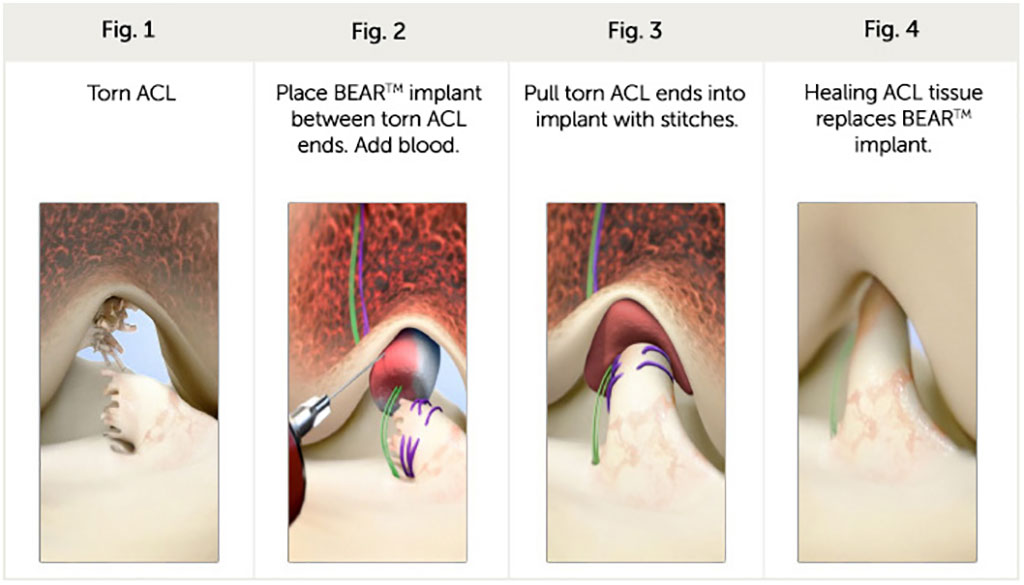
Image: An ECM implant repairs a torn ACL (Photo courtesy of Miach Orthopaedics)
A novel implant acts as a biological bridge between the two ends of a torn anterior cruciate ligament (ACL) to facilitate healing.
The Miach Orthopaedics (Westborough, MA, USA) Bridge-Enhanced ACL Repair (BEAR) implant is designed to restore natural anatomy and function of the knee. The implant, which is comprised of a proprietary blend of extracellular matrix (ECM) proteins and collagen, is stitched into place during arthroscopy between the torn ends of the ACL and then injected with the patient’s blood, which clots in the implant. The BEAR is held in place long enough for the body to heal the torn ends of the ACL back together, while maintaining its original attachments to the femur and tibia. As the ACL heals, the BEAR implant is absorbed by the body, within approximately eight weeks.
Unlike surgical ACL reconstruction, which is the current standard of care, the implant does not require a second surgical wound site to remove a healthy tendon from another part of the leg, or implanting a deceased donor's tendon. The BEAR implant is indicated for skeletally mature patients at least 14 years of age with a complete rupture of the ACL, as confirmed by magnetic resonance imaging (MRI). Patients must have an ACL stump attached to the tibia to construct the repair, and the device must be implanted within 50 days of injury.
“Preserving a patient's native ACL instead of replacing it with a graft has long been a goal of surgeons, and before the BEAR implant, multiple approaches were studied and failed,” said Martha Shadan, CEO and president of Miach Orthopaedics. “The BEAR implant, which is the first medical technology to show that it enables a patient's own torn ACL to heal, represents the first substantial advancement in the treatment of ACL tears in decades, and has the potential to change the standard of care.”
The ACL is a broad, thick collagen cord that originates on the anterior portion of the femur in the intercondylar notch and inserts on the posterior aspect of the tibial plateau. The ACL guides the tibia through a normal, stable range of motion, along the end of the femur, maintaining joint stability. The ligament is unfortunately poorly vascularized, and thus has no ability to heal itself after a complete tear, leading to further destruction of the articular and meniscal cartilage over time.
Related Links:
Miach Orthopaedics
The Miach Orthopaedics (Westborough, MA, USA) Bridge-Enhanced ACL Repair (BEAR) implant is designed to restore natural anatomy and function of the knee. The implant, which is comprised of a proprietary blend of extracellular matrix (ECM) proteins and collagen, is stitched into place during arthroscopy between the torn ends of the ACL and then injected with the patient’s blood, which clots in the implant. The BEAR is held in place long enough for the body to heal the torn ends of the ACL back together, while maintaining its original attachments to the femur and tibia. As the ACL heals, the BEAR implant is absorbed by the body, within approximately eight weeks.
Unlike surgical ACL reconstruction, which is the current standard of care, the implant does not require a second surgical wound site to remove a healthy tendon from another part of the leg, or implanting a deceased donor's tendon. The BEAR implant is indicated for skeletally mature patients at least 14 years of age with a complete rupture of the ACL, as confirmed by magnetic resonance imaging (MRI). Patients must have an ACL stump attached to the tibia to construct the repair, and the device must be implanted within 50 days of injury.
“Preserving a patient's native ACL instead of replacing it with a graft has long been a goal of surgeons, and before the BEAR implant, multiple approaches were studied and failed,” said Martha Shadan, CEO and president of Miach Orthopaedics. “The BEAR implant, which is the first medical technology to show that it enables a patient's own torn ACL to heal, represents the first substantial advancement in the treatment of ACL tears in decades, and has the potential to change the standard of care.”
The ACL is a broad, thick collagen cord that originates on the anterior portion of the femur in the intercondylar notch and inserts on the posterior aspect of the tibial plateau. The ACL guides the tibia through a normal, stable range of motion, along the end of the femur, maintaining joint stability. The ligament is unfortunately poorly vascularized, and thus has no ability to heal itself after a complete tear, leading to further destruction of the articular and meniscal cartilage over time.
Related Links:
Miach Orthopaedics
Latest Surgical Techniques News
- Early TAVR Intervention Reduces Cardiovascular Events in Asymptomatic Aortic Stenosis Patients
- New Procedure Found Safe and Effective for Patients Undergoing Transcatheter Mitral Valve Replacement
- No-Touch Vein Harvesting Reduces Graft Failure Risk for Heart Bypass Patients
- DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
- Tiny Robotic Tools Powered by Magnetic Fields to Enable Minimally Invasive Brain Surgery
- Magnetic Tweezers Make Robotic Surgery Safer and More Precise
- AI-Powered Surgical Planning Tool Improves Pre-Op Planning
- Novel Sensing System Restores Missing Sense of Touch in Minimally Invasive Surgery
- Headset-Based AR Navigation System Improves EVD Placement
Channels
Critical Care
view channel
AI Interpretability Tool for Photographed ECG Images Offers Pixel-Level Precision
The electrocardiogram (ECG) is a crucial diagnostic tool in modern medicine, used to detect heart conditions such as arrhythmias and structural abnormalities. Every year, millions of ECGs are performed... Read more
AI-ECG Tools Can Identify Heart Muscle Weakness in Women Before Pregnancy
Each year, some mothers die from heart-related issues after childbirth, with many of these deaths being preventable. Screening for heart weakness before pregnancy could be crucial in identifying women... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more