Screening for Atrial Fibrillation Using Smartphones More Than Doubles Detection Rate
|
By HospiMedica International staff writers Posted on 02 Sep 2022 |

Atrial fibrillation is the most common heart rhythm disorder, affecting more than 40 million people worldwide. Those affected have a five times greater risk of stroke than their peers. Atrial fibrillation often has no symptoms and remains undiagnosed, leaving patients unprotected from stroke. Prior studies have shown the potential of smart devices for large-scale atrial fibrillation screening but they made no comparison with conventional screening, included primarily younger adults for whom screening has low relevance, and required participants to own certain hardware. It has been unclear to what extent older adults, who would benefit most from screening, could cope with digital technologies and whether screening results in initiation of oral anticoagulation. Now, a new study has shown that atrial fibrillation screening using conventional smartphones more than doubles the detection and treatment rate in older people compared to routine screening.
Researchers at Innsbruck Medical University (Innsbruck, Austria) conducted a site-less randomized study in older adults at risk for stroke who owned a smartphone. Smartphone screening was compared with usual screening for the ability to detect atrial fibrillation that was then treated with oral anticoagulation. Policyholders with a large healthcare insurance company were invited to participate if they fulfilled these criteria: age 50 to 90 years, no known atrial fibrillation, no prescription of oral anticoagulants, and a CHA2DS2-VASc score ≥1 (men; ≥2 in women). A dedicated study app was used by the researchers to check inclusion criteria and trigger randomization, and to initiate a crossover phase. Participants used the app to answer questionnaires.
The trial enrolled 5,551 of 67,488 invited policyholders. The median age of participants was 65 years and 31% were women. Participants were randomly assigned to a six-month digital or conventional atrial fibrillation screening strategy. Those in the digital arm downloaded a certified app to their own smartphone that measures pulse wave irregularities using the phone's photoplethysmographic (PPG) sensor. To start a one-minute PPG measurement, participants placed their finger on the smartphone's camera. Participants were instructed to measure twice a day for 14 days, then twice a week – push notifications were used as reminders. In case of abnormal results, participants were posted a patch to record a 14-day ECG which they then returned by post. The researchers evaluated the ECG, sent the results to participants and asked them to consult their local physician, who made the treatment decision and was not involved in the study.
The conventional arm reflected atrial fibrillation screening in real world practice which can be by symptoms, routine ECG screening, and other methods. In both groups, information on newly detected atrial fibrillation was collected by the researchers via app-based questionnaires, telephone calls as well as insurance claims data. A total of 2,860 participants were assigned to digital screening and 2,691 participants were assigned to conventional screening. The primary efficacy endpoint was newly diagnosed atrial fibrillation within six months leading to initiation of oral anticoagulation by an independent physician. The primary endpoint occurred in 38 participants (1.33%) in the digital arm and 17 (0.63%) in the conventional arm, for an odds ratio (OR) of 2.12 (95% confidence interval [CI] 1.19–3.76; p=0.010).
Those who did not reach the primary endpoint in the first six months were invited to take part in a second six-month study phase with crossover assignment to conventional or digital screening, respectively. This gave all participants the opportunity to undergo digital screening, increased the statistical power for secondary analyses, and enabled validation of the primary results. A total of 4,752 (85.6%) participants crossed over and entered the second study phase. Again, digital screening was superior to conventional screening in detecting atrial fibrillation that was then treated with oral anticoagulation (33 of 2,387 versus 12 of 2,365 participants; OR 2.95; 95% CI 1.52–5.72; p=0.001). In secondary analyses, atrial fibrillation, PPG-detected atrial fibrillation, and abnormal PPG findings significantly predicted major adverse cardiac and cerebrovascular events (MACCE), with hazard ratios of 6.13 (95% CI 3.07–12.21; p<0.001), 3.22 (95% CI 1.01–10.33; p=0.049) and 2.74 (95% CI 1.25–6.00; p=0.012), respectively.
“Screening using common smartphones significantly increased the detection rate of therapy-relevant atrial fibrillation. Importantly, app-based pre-screening was only one part of the programme, which also included electrocardiogram (ECG) validation and assessment of the findings by an independent physician,” said Professor Axel Bauer of Innsbruck Medical University. “This trial focused on a target population for atrial fibrillation screening, rather than all-comers. We found that digital screening was well received by older participants, who tended to perform even more PPG measurements than younger participants in the study. Digitally detected atrial fibrillation as well as abnormal PPG measurements per se were of prognostic significance as they predicted MACCE.”
Related Links:
Innsbruck Medical University
Latest Critical Care News
- Novel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
- Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
- Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
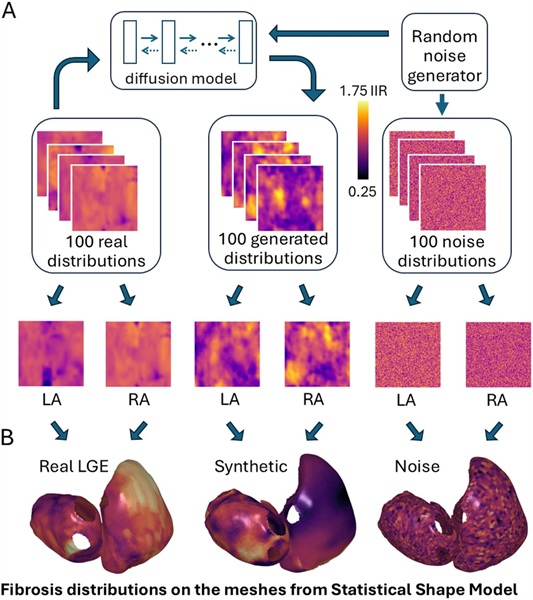
- Generative AI Technology Detects Heart Disease Earlier Than Conventional Methods
- Wearable Technology Predicts Cardiovascular Risk by Continuously Monitoring Heart Rate Recovery
- Wearable Health Monitoring Device Measures Gases Emitted from and Absorbed by Skin
- Groundbreaking Technology Rapidly Detects Airborne Influenza Viruses
- Handheld Device Could Transform Heart Disease Screening
- Flexible Semi-Autonomous Robot Could Deliver Medicine Inside Body

- Neurorestorative Treatment Strategies Hold Promise for Most Severe Forms of Epilepsy
- Gene Discovery Could Help Grow New Heart Arteries
- Study Discovers Invisible Transmission of Common Hospital-Associated Infection
- Non-Invasive Neuro-Ophthalmology Techniques Could Detect Brain Tumors Earlier
- Mass Manufactured Nanoparticles to Deliver Cancer Drugs Directly to Tumors
- World’s Smallest Pacemaker Fits Inside Syringe Tip

- AI-Powered, Internet-Connected Medical Devices to Revolutionize Healthcare, Finds Study
Channels
Surgical Techniques
view channel
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more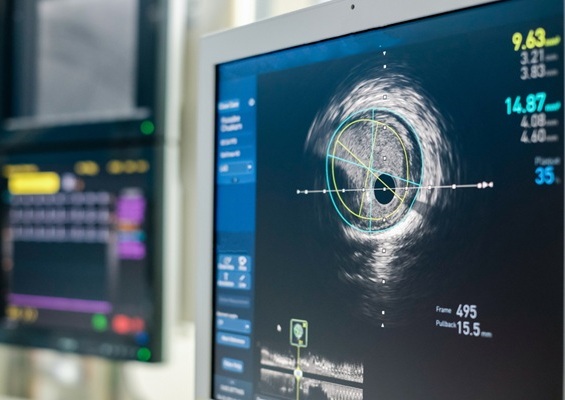
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more