World’s Smallest Implantable Brain Stimulator Demonstrated in Human Patient 
|
By HospiMedica International staff writers Posted on 15 Apr 2024 |

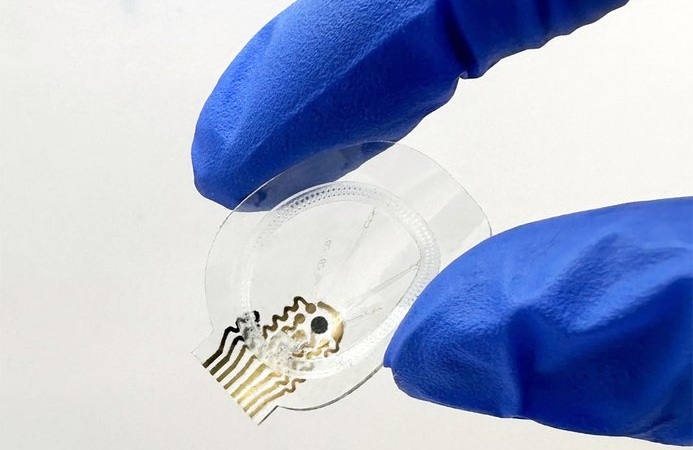
Implantable devices that deliver electrical stimulation to the central or peripheral nervous system are increasingly employed in the treatment of psychiatric conditions, movement disorders, and pain issues, and for helping to restore mobility after spinal cord injuries. However, the current implantable devices used for brain stimulation depend on comparatively large batteries. These batteries need to be implanted under the skin at a location different from the stimulation device and are connected by long wires. This arrangement requires additional surgeries, increases the risk of hardware complications like wire breakage, and often requires surgeries to replace batteries. Engineers have now developed what is considered the smallest implantable brain stimulator used in a human to date. Utilizing innovative magnetoelectric power transfer technology, this tiny device can be wirelessly powered by an external transmitter and is capable of stimulating the brain through the dura—the protective membrane that lines the base of the skull.
This device, created by engineers at Rice University (Houston, TX, USA) and dubbed the Digitally programmable Over-brain Therapeutic (DOT), could transform the treatment landscape for drug-resistant depression and other psychiatric or neurological disorders. It provides a less invasive alternative compared to existing neurostimulation therapies and other brain-computer interfaces (BCIs), offering greater patient autonomy and easier access. The device utilizes a material that efficiently converts magnetic fields into electrical energy. This conversion is highly efficient even at small dimensions and tolerates alignment errors well, simplifying the activation and control processes. The device itself is 9 millimeters wide and capable of delivering up to 14.5 volts of electrical stimulation.
In initial tests, the device was temporarily implanted in a human patient to stimulate the motor cortex, the brain region that controls movement, successfully eliciting a hand movement. Further tests showed that the device could stably interface with the brain for up to 30 days in pig models. The implant procedure, taking about 30 minutes, involves placing the device within the skull bone, resulting in an almost invisible incision and implant site. Patients would be able to return home on the same day as the procedure. The technology could allow it to be operated comfortably from home. Doctors would prescribe and oversee the treatment, but patients would manage the application themselves.
“In the future, we can place the implant above other parts of the brain, like the prefrontal cortex, where we expect to improve executive functioning in people with depression or other disorders,” said Jacob Robinson, a professor of electrical and computer engineering and of bioengineering at Rice.
Related Links:
Rice University
Latest Surgical Techniques News
- DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
- Tiny Robotic Tools Powered by Magnetic Fields to Enable Minimally Invasive Brain Surgery
- Magnetic Tweezers Make Robotic Surgery Safer and More Precise
- AI-Powered Surgical Planning Tool Improves Pre-Op Planning
- Novel Sensing System Restores Missing Sense of Touch in Minimally Invasive Surgery
- Headset-Based AR Navigation System Improves EVD Placement
- Higher Electrode Density Improves Epilepsy Surgery by Pinpointing Where Seizures Begin
- Open-Source Tool Optimizes Placement of Visual Brain Implants
- Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
Channels
Critical Care
view channel
Breakthrough AI Technology Accurately Assesses Heart Failure Severity
Heart failure (HF) is a complex condition where the heart cannot effectively pump blood to meet the body’s needs due to underlying medical issues. It is marked by recurring episodes and frequent hospitalizations.... Read more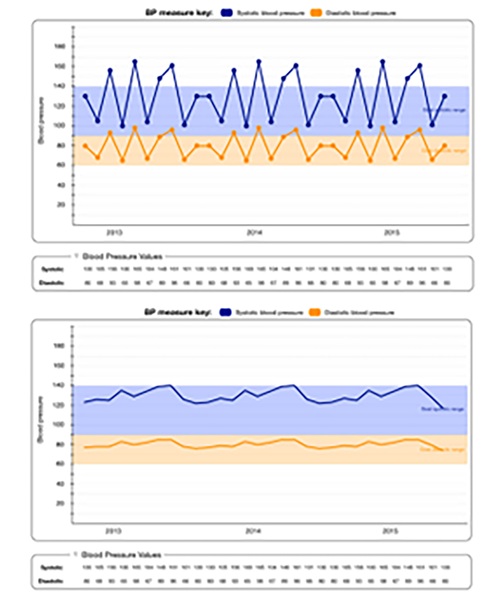
New Approach to Visualizing Blood Pressure Data Can Help Better Manage Hypertension Patients
Sometimes, a patient’s blood pressure may be elevated in a doctor's office but normal at home, a phenomenon known as white coat hypertension. It is estimated that 10% to 20% of high blood pressure diagnoses... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more