New Guideline Details Management of CVD Risk Before, During and After Noncardiac Surgery
|
By HospiMedica International staff writers Posted on 07 Oct 2024 |
_1.jpg)
There are approximately 300 million noncardiac surgeries performed worldwide each year, highlighting the importance of summarizing and interpreting evidence to help clinicians manage patients undergoing surgery. The American Heart Association (AHA, Dallas, TX, USA) and the American College of Cardiology (ACC, Washington, DC, USA) have now released an updated joint guideline on cardiovascular evaluation and management for patients before, during, and after noncardiac surgery. This guideline reviews a decade of new evidence and provides updates since the previous version was released in 2014.
Published in the AHA’s flagship, peer-reviewed journal Circulation and simultaneously in JACC, the flagship journal of the ACC, the “2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM Guideline for Perioperative Cardiovascular Management for Noncardiac Surgery” presents the latest evidence for assessing and managing cardiovascular disease risk in patients scheduled for noncardiac surgery. It addresses patient evaluations, cardiovascular testing, screening, and evidence-based management of cardiovascular conditions before, during, and after surgery. The guideline is aimed at healthcare professionals from multiple disciplines who care for patients undergoing surgeries requiring general or regional anesthesia and who may have known or potential cardiovascular risks.
As in the 2014 guideline, the 2024 update includes a perioperative algorithm to guide healthcare professionals in making care decisions for patients with cardiovascular conditions who are undergoing noncardiac surgery. It reviews blood pressure management and includes specific recommendations for patients with coronary artery disease, hypertrophic cardiomyopathy, valvular heart disease, pulmonary hypertension, obstructive sleep apnea, and those with a history of stroke. The new guideline advises a targeted approach when ordering screenings, such as stress tests, to assess cardiac risk before surgery. Additionally, it recommends the use of emergency-focused cardiac ultrasound for patients with unexplained hemodynamic instability during noncardiac surgery, provided clinicians skilled in cardiac ultrasound are available. This ultrasound technology, which has become a screening option since the last guideline, can be used during surgery to determine whether heart problems are causing unstable blood pressure.
The 2024 guideline also highlights newer medications for Type 2 diabetes, heart failure, and obesity management that have significant perioperative implications. For example, SGLT2 inhibitors should be discontinued three to four days before surgery to reduce the risk of perioperative ketoacidosis, which can negatively impact surgical outcomes. Additionally, emerging data suggest that glucagon-like polypeptide-1 (GLP-1) agonists, used to manage Type 2 diabetes and obesity, may delay stomach emptying and increase the risk of pulmonary aspiration during anesthesia due to their side effect of nausea. Other medical organizations have recommended withholding GLP-1 agonists before noncardiac surgery—one week for patients on weekly doses and one day for those on daily doses—to mitigate this risk, though further research is needed to refine these recommendations. For patients taking blood thinners, the guideline suggests that, in most cases, it is safe to stop the medication several days before surgery and restart it after surgery, typically after hospital discharge. Exceptions and modifications to this recommendation are also outlined in the guideline.
Another focus of the new guideline is myocardial injury after noncardiac surgery (MINS), which refers to heart damage occurring during or shortly after noncardiac surgery. MINS, diagnosed by elevated cardiac troponin levels, affects roughly one in five patients and is associated with worse short- and long-term outcomes. While the causes and management strategies for MINS remain unclear, the guideline recommends outpatient follow-up for patients who develop this condition to reduce heart disease risk factors. Additionally, the guideline emphasizes the need to monitor atrial fibrillation (AFib), an irregular heart rhythm that can develop during or after noncardiac surgery. Patients newly diagnosed with AFib are at an increased risk of stroke, and the guideline advises close monitoring of these patients after surgery, addressing reversible causes of AFib and considering rhythm control or the use of blood thinners to prevent stroke. Ongoing studies are investigating the best ways to manage AFib that occurs postoperatively.
“There is a wealth of new evidence about how best to evaluate and manage perioperative cardiovascular risk in patients undergoing noncardiac surgery,” said Chair of the guideline writing group Annemarie Thompson, M.D., M.B.A., FAHA. “This new guideline is a comprehensive review of the latest research to help inform clinicians who manage perioperative patients, with the ultimate goal of restoring health and minimizing cardiovascular complications.”
Latest Critical Care News
- AI Model Analyzes Patient Data to Diagnose Multiple Sclerosis With 90% Accuracy
- Magnetically Navigable Microparticles Enable Targeted Drug Delivery
- AI-Powered Algorithm Automates Analysis of Coronary Stents After Implantation
- New Stroke Risk Scoring System to Help Avoid Unnecessary Surgeries
- Wearable Device Tracks Individual Cells in Bloodstream in Real Time
- Drug Delivery System Uses Ultrasound-Activated Nanoparticles to Destroy Bacterial Biofilms
- New Potent Injectable Therapy Could Prevent Heart Failure After Heart Attack
- Hospital-Based System Combines AI and Genomic Surveillance to Quickly Detect Infectious Disease Outbreaks
- New Approach to Visualizing Blood Pressure Data Can Help Better Manage Hypertension Patients
- Breakthrough AI Technology Accurately Assesses Heart Failure Severity
- Smart Bandage Monitors Chronic Wounds in Human Patients
- AI Identifies Patients with Increased Lung Cancer Risk Up To 4 Months Earlier
- Next Gen Hemodynamic Monitoring Solution Provides AI-Driven Clinical Decision Support
- AI Algorithm Identifies High-Risk Heart Patients
- Wearable Glucose Monitor Offers Less Invasive Approach to Assessing Diabetes Risk
- Wireless, Self-Powered Smart Insole to Improve Personal Health Monitoring
Channels
Surgical Techniques
view channel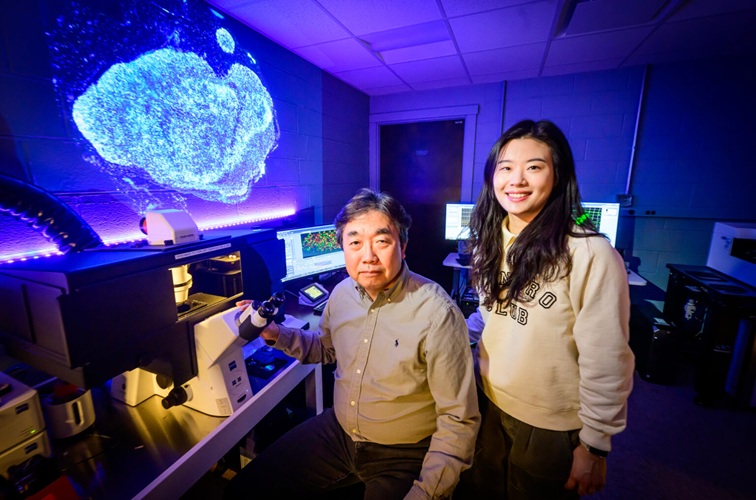
DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
One of the challenges of fighting pancreatic cancer is finding ways to penetrate the organ’s dense tissue to define the margins between malignant and normal tissue. Now, a new study uses DNA origami structures... Read more
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more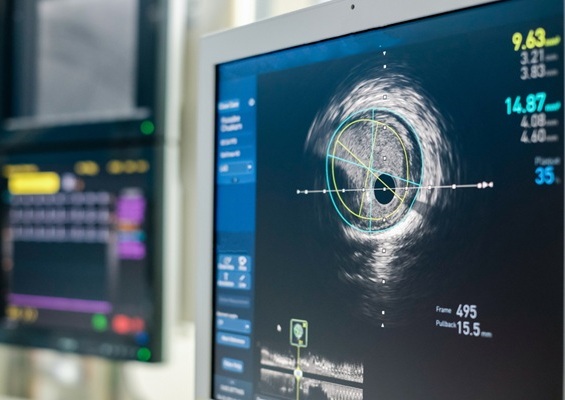
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more















