Electronic Diagnostic Model Predicts Acute Interstitial Nephritis in Patients
|
By HospiMedica International staff writers Posted on 15 Nov 2024 |
Acute interstitial nephritis (AIN) is a frequent cause of acute kidney injury (AKI), characterized by inflammation and swelling of certain kidney tissues. It is typically associated with the use of medications such as steroids, proton pump inhibitors, and antibiotics. Studies show that AKI, which involves a sudden decline in kidney function, affects about 20% of hospitalized patients. One of the key challenges in managing AKI is distinguishing AIN from other causes of kidney injury. This is complicated by the fact that over 90% of AIN patients show no obvious symptoms, and common diagnostic methods, including urine eosinophil counts, urine microscopy, and imaging tests, have poor accuracy. Misdiagnosing AIN can result in the premature discontinuation of essential treatments like immune checkpoint inhibitors or antibiotics, potentially leading to permanent kidney damage if the condition is not promptly identified. Given the difficulty of diagnosing AIN, a kidney biopsy is often required, though it is an invasive procedure with its own risks. To address this challenge, researchers have developed a diagnostic model using lab tests from electronic medical records, which could significantly improve early detection of AIN in patients.
In the study, researchers from Johns Hopkins Medicine (Baltimore, MD, USA) and Yale University (New Haven, CT, USA) developed a diagnostic model to predict AIN in patients using a machine learning technique called least absolute shrinkage and selection operator (LASSO). The laboratory tests used in the model included serum creatinine, blood urea nitrogen (BUN), urine protein levels, and urine specific gravity (the density of urine compared to water). The study involved two patient cohorts, both of which had previously undergone kidney biopsies at Johns Hopkins Hospital (JHH) or Yale University. The JHH cohort consisted of 1,454 patients who had a native kidney biopsy between January 2019 and December 2022, while the Yale cohort included 528 patients scheduled for clinical kidney biopsy between July 2020 and June 2023. Patients who did not have a serum creatinine value within a year before their biopsy, were undergoing kidney allograft biopsies, or had known vasculitis or lupus nephritis were excluded from the study.
A total of 1,982 patients were analyzed, with 22% diagnosed with AIN. The study found that patients with AIN were more likely to be hospitalized and had higher serum creatinine levels and a higher blood urea nitrogen-to-creatinine ratio. The diagnostic model improved the accuracy of AIN diagnosis to 77%. However, there were differences in the prevalence of AIN between the two cohorts. After adjusting for prevalence at the individual centers, the model's calibration improved significantly, leading to more accurate diagnoses. The findings, published in the Journal of the American Society of Nephrology, suggest that this diagnostic model could assist clinicians in determining whether a kidney biopsy is necessary in patients with AKI and help guide treatment decisions for AIN. The formula for predicting AIN is available on MDCalc.
Latest Critical Care News
- Smart Bandage Monitors Chronic Wounds in Human Patients
- AI Identifies Patients with Increased Lung Cancer Risk Up To 4 Months Earlier
- Next Gen Hemodynamic Monitoring Solution Provides AI-Driven Clinical Decision Support
- AI Algorithm Identifies High-Risk Heart Patients
- Wearable Glucose Monitor Offers Less Invasive Approach to Assessing Diabetes Risk
- Wireless, Self-Powered Smart Insole to Improve Personal Health Monitoring
- Novel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
- Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
- Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
- Generative AI Technology Detects Heart Disease Earlier Than Conventional Methods
- Wearable Technology Predicts Cardiovascular Risk by Continuously Monitoring Heart Rate Recovery
- Wearable Health Monitoring Device Measures Gases Emitted from and Absorbed by Skin
- Groundbreaking Technology Rapidly Detects Airborne Influenza Viruses
- Handheld Device Could Transform Heart Disease Screening
- Flexible Semi-Autonomous Robot Could Deliver Medicine Inside Body

- Neurorestorative Treatment Strategies Hold Promise for Most Severe Forms of Epilepsy
Channels
Surgical Techniques
view channel
DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
One of the challenges of fighting pancreatic cancer is finding ways to penetrate the organ’s dense tissue to define the margins between malignant and normal tissue. Now, a new study uses DNA origami structures... Read more
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more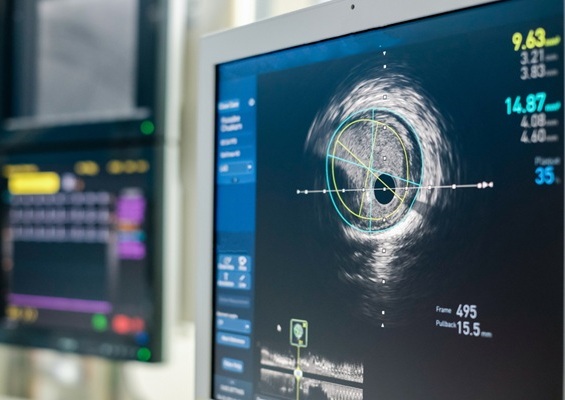
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more















