Activating T Cells Could Improve Neurological Outcomes After Cardiac Arrest
|
By HospiMedica International staff writers Posted on 06 Dec 2024 |

Despite advancements in cardiopulmonary resuscitation (CPR) and improved hospital access, survival rates after out-of-hospital cardiac arrest (OHCA) remain low, with only about 10% of patients surviving. After reaching the hospital, most individuals who survive the initial cardiac arrest succumb to brain injury, and there are currently no medications available to prevent this outcome. Researchers have now identified a specific group of cells that could potentially offer protection against brain damage following cardiac arrest, prompting them to explore a drug that activates these cells to improve neurological recovery.
A team of researchers from Mass General Brigham (Somerville, MA, USA) studied samples from OHCA patients and discovered changes in immune cells just six hours after cardiac arrest that could predict brain recovery 30 days later. They identified a particular population of cells that might offer protection from brain injury and a drug that can activate these cells, which they tested in preclinical models. The research followed their observation that while some cardiac arrest patients showed elevated inflammation during their first night in the hospital, they showed rapid improvement thereafter. In contrast, other patients continued to deteriorate and eventually died. To understand why some patients survived while others did not, the team began collecting a biobank of cryopreserved cells, donated by patients with consent from their families, just hours after their cardiac arrest. Using single-cell transcriptomics, they examined gene activity in the cells.
The findings, published in Science Translational Medicine, revealed that one group of cells, called diverse natural killer T (dNKT) cells, was elevated in patients who showed favorable neurological recovery. These cells seemed to play a protective role in preventing brain injury. To further explore this, the team treated mice with sulfatide lipid antigen, a drug that activates these protective NKT cells, following cardiac arrest. The mice demonstrated improved neurological outcomes. While the researchers acknowledge the limitations of mouse models, they believe that insights from human samples first could enhance the likelihood of successfully translating their findings into effective treatments for patients. Additional preclinical studies are necessary, but their ultimate goal is to move toward clinical trials to determine if the drug can protect against brain injury when administered soon after cardiac arrest.
“Cardiac arrest outcomes are grim, but I am optimistic about jumping into this field of study because, theoretically, we can treat a patient at the moment injury happens,” said co-senior and corresponding author Edy Kim, MD, PhD, of the Division of Pulmonary and Critical Care Medicine at Brigham and Women’s Hospital. “This represents a completely new approach, activating T cells to improve neurological outcomes after cardiac arrest. And a fresh approach could lead to life-changing outcomes for patients.”
Latest Critical Care News
- Novel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
- Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
- Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
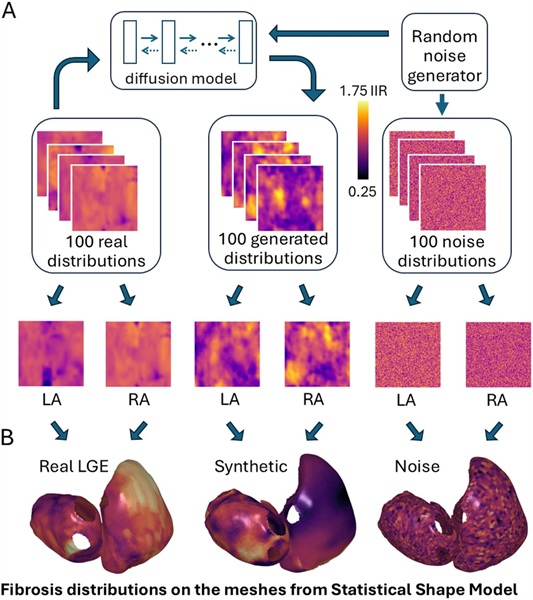
- Generative AI Technology Detects Heart Disease Earlier Than Conventional Methods
- Wearable Technology Predicts Cardiovascular Risk by Continuously Monitoring Heart Rate Recovery
- Wearable Health Monitoring Device Measures Gases Emitted from and Absorbed by Skin
- Groundbreaking Technology Rapidly Detects Airborne Influenza Viruses
- Handheld Device Could Transform Heart Disease Screening
- Flexible Semi-Autonomous Robot Could Deliver Medicine Inside Body

- Neurorestorative Treatment Strategies Hold Promise for Most Severe Forms of Epilepsy
- Gene Discovery Could Help Grow New Heart Arteries
- Study Discovers Invisible Transmission of Common Hospital-Associated Infection
- Non-Invasive Neuro-Ophthalmology Techniques Could Detect Brain Tumors Earlier
- Mass Manufactured Nanoparticles to Deliver Cancer Drugs Directly to Tumors
- World’s Smallest Pacemaker Fits Inside Syringe Tip

- AI-Powered, Internet-Connected Medical Devices to Revolutionize Healthcare, Finds Study
Channels
Surgical Techniques
view channel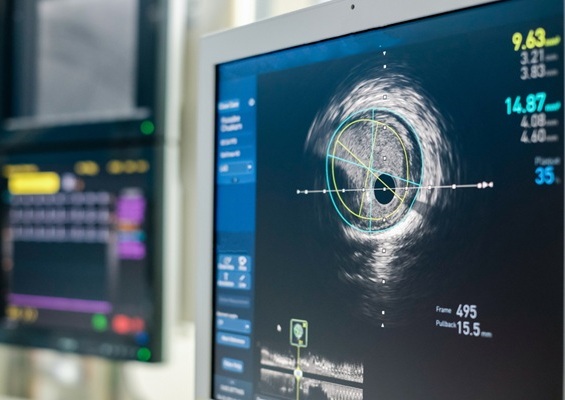
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more