AI-Powered Imaging Technique Shows Promise in Evaluating Patients for PCI
|
By HospiMedica International staff writers Posted on 01 Apr 2025 |
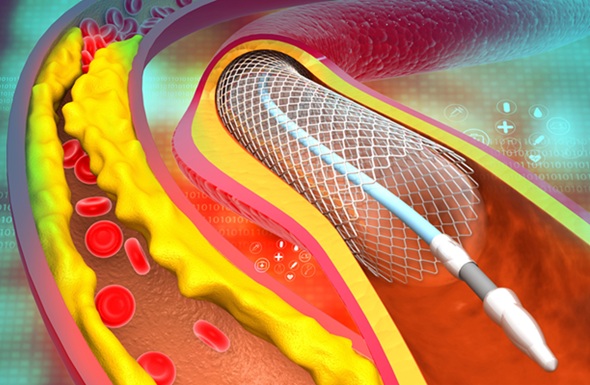
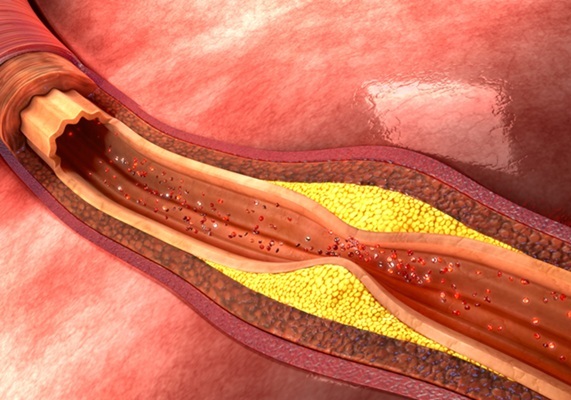
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a minimally invasive procedure where small metal tubes called stents are inserted into partially blocked coronary arteries to help keep them open. To determine which patients are most likely to benefit from PCI, fractional flow reserve (FFR) assessment is used. This technique measures blood pressure and flow in the blocked arteries, helping identify which patients should undergo PCI and which ones can be managed with medication. Typically, patients with an FFR score of 0.80 or lower are recommended for PCI, while those with a score above 0.80 continue with medication. Traditional FFR assessment involves threading a catheter or wire through the body to assess blood flow and pressure in the coronary arteries. While effective in identifying those most likely to benefit from PCI, technical and logistical challenges have hindered the widespread use of this method. Now, researchers have found that patients with at least 50% narrowing in three major coronary arteries had similar outcomes when treated with a minimally invasive stent placement guided by either ultrasound-based imaging or a novel, artificial intelligence (AI)-powered non-invasive imaging method derived from angiography.
The FLAVOUR II study, conducted by researchers from The Second Affiliated Hospital of Zhejiang University School of Medicine (Hangzhou, China), aimed to assess the effectiveness of AI-powered FFR assessment in PCI outcomes. The study met its primary endpoint, which combined death, heart attack, or the need for a repeat procedure after one year. The study enrolled patients who had angiographically significant coronary artery disease, with three of the major arteries supplying blood to the heart showing inflammation or partial blockage from cholesterol buildup. The patients experienced symptoms such as chest pain and shortness of breath. The research team used an innovative AI method called AngioFFR, which calculates FFR from a single-view angiogram (X-ray) of the coronary arteries. Unlike conventional FFR assessment, AngioFFR is non-invasive, simpler, and quicker to perform. The study aimed to compare the outcomes of patients receiving PCI guided by AngioFFR with those guided by intravascular ultrasound (IVUS), which uses sound waves to visualize the extent of arterial narrowing and is the most common imaging technique for guiding PCI.
A total of 1,872 patients (average age 65 years, 68% male) from 22 medical centers in China participated in the study. To be eligible, patients needed at least 50% narrowing in three major coronary arteries, without significant narrowing in the left main coronary artery. Many of the participants had one or more co-existing conditions, including high blood pressure (67.6%), diabetes (31%), high cholesterol (66.9%), chronic kidney disease (24.3%), smoking (25%), and previous heart attack (13.9%). Participants were randomly assigned to undergo either AngioFFR-guided or IVUS-guided PCI. In the AngioFFR group, PCI was performed if the AngioFFR score was 0.80 or lower. In the IVUS group, PCI was carried out if the narrowest part of the artery was between three and four millimeters in width, and the plaque burden (the amount of plaque in the most severely narrowed part of the artery) was above 70%.
At the one-year follow-up, 73.9% of patients in the AngioFFR group received PCI, compared to 83.1% in the IVUS group. The rate of composite outcomes, including death, heart attack, or the need for a repeat procedure, was 6.3% in the AngioFFR group and 6.0% in the IVUS group, with no significant statistical difference. The clinical outcomes of both groups in terms of death, heart attack, and the need for a repeat procedure were similar. The researchers also observed no significant differences between the groups in subgroups such as patients with diabetes. The team plans to continue following the study participants for at least five years to assess any long-term differences in effectiveness between the two methods. The results were presented at the American College of Cardiology’s Annual Scientific Session (ACC.25) and published simultaneously online in The Lancet. However, the researchers acknowledged the study's limitations, including the lack of complex lesions among participants, which are more challenging to treat with PCI, and the lack of diversity in the patient population, as the study was conducted in China.
“This is the first such study to be conducted in patients with angiographically significant lesions,” said Jian’an Wang, MD, a professor in the Heart Center at The Second Affiliated Hospital of Zhejiang University School of Medicine, and the study’s senior author. “Patients whose evaluation was non-invasively guided by the novel, AI-powered technique underwent approximately 10% fewer procedures, and their outcomes were comparable with those for patients whose evaluation was guided by a commonly used ultrasound-based imaging technique.”
Latest Surgical Techniques News
- DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
- Tiny Robotic Tools Powered by Magnetic Fields to Enable Minimally Invasive Brain Surgery
- Magnetic Tweezers Make Robotic Surgery Safer and More Precise
- AI-Powered Surgical Planning Tool Improves Pre-Op Planning
- Novel Sensing System Restores Missing Sense of Touch in Minimally Invasive Surgery
- Headset-Based AR Navigation System Improves EVD Placement
- Higher Electrode Density Improves Epilepsy Surgery by Pinpointing Where Seizures Begin
- Open-Source Tool Optimizes Placement of Visual Brain Implants
- Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
Channels
Critical Care
view channel
AI Model Analyzes Patient Data to Diagnose Multiple Sclerosis With 90% Accuracy
Multiple sclerosis (MS) is a chronic inflammatory condition affecting the central nervous system. Most patients initially experience the relapsing-remitting form (RRMS), characterized by periods of symptom... Read more
Magnetically Navigable Microparticles Enable Targeted Drug Delivery
Abdominal aortic aneurysms (AAA) can be life-threatening if not treated and result in nearly 10,000 deaths annually. Researchers working to improve treatments for AAA could now make it possible for doctors... Read more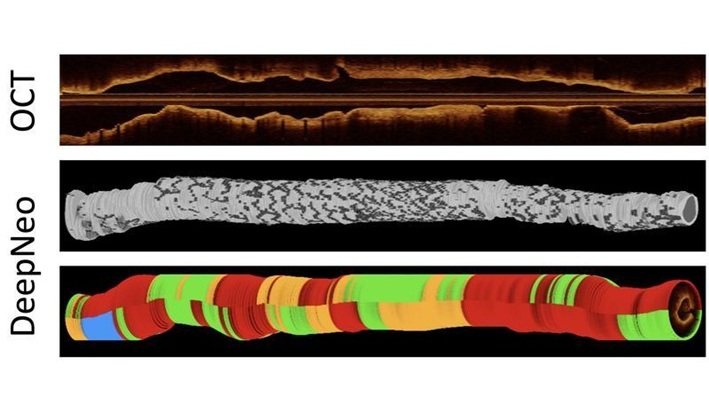
AI-Powered Algorithm Automates Analysis of Coronary Stents After Implantation
Every year, over three million people globally receive stents to open blocked blood vessels caused by heart disease. However, monitoring the healing process after stent implantation remains a significant challenge.... Read moreSurgical Techniques
view channel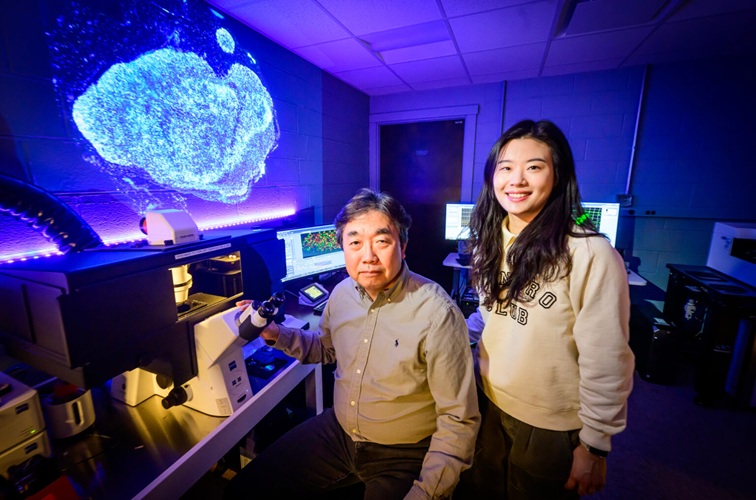
DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
One of the challenges of fighting pancreatic cancer is finding ways to penetrate the organ’s dense tissue to define the margins between malignant and normal tissue. Now, a new study uses DNA origami structures... Read more
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more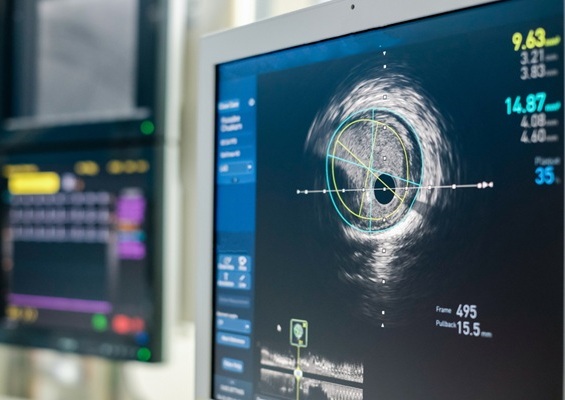
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more