World’s Smallest Pacemaker Fits Inside Syringe Tip
|
By HospiMedica International staff writers Posted on 04 Apr 2025 |
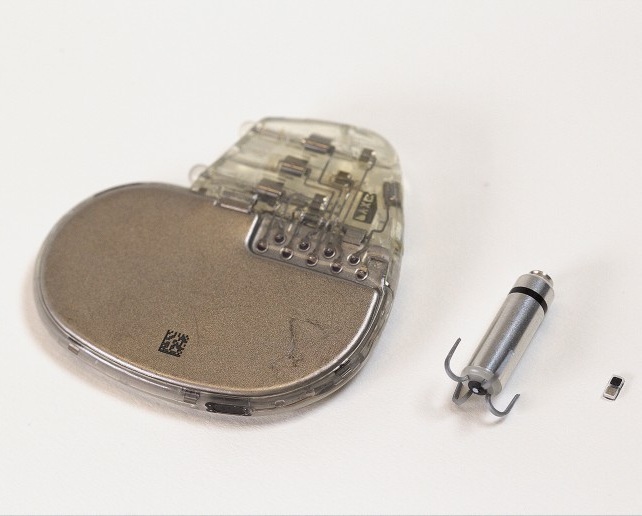
After heart surgery, many patients require temporary pacemakers either to regulate the heart rate while waiting for a permanent pacemaker or to support normal heart rhythm during recovery. The current standard of care involves surgeons attaching electrodes to the heart muscle during surgery. Wires from these electrodes exit the chest and connect to an external pacing device, which delivers current to control the heart's rhythm. Once the temporary pacemaker is no longer necessary, the electrodes are removed. However, this process can lead to complications such as infections, dislodgement, tissue damage, bleeding, and blood clots. In response to these challenges, engineers have developed a pacemaker small enough to fit inside a syringe, allowing it to be non-invasively injected into the body. This pacemaker is designed for temporary use, particularly benefiting newborn babies with congenital heart defects and those with small, fragile hearts.
Developed by engineers at Northwestern University (Evanston, IL, USA), this pacemaker is smaller than a grain of rice and is paired with a soft, flexible, wireless, wearable device. This device mounts on the patient's chest and controls the pacemaker. When it detects an irregular heartbeat, the wearable emits a pulse of light, activating the pacemaker. These light pulses penetrate the patient’s skin, muscles, and breastbone to control the pacing. The pacemaker dissolves once it is no longer needed, as all components are biocompatible and dissolve harmlessly in the body’s biofluids, eliminating the need for surgical removal. This innovative device's effectiveness has been demonstrated across large and small animal models and human hearts from deceased organ donors, with findings published in the journal Nature.
This research builds on earlier work by the team, which first developed a dissolvable device for temporary pacing. In that earlier study, the team introduced a flexible, lightweight, bioresorbable pacemaker that removed the need for bulky batteries, rigid hardware, and wires. The concept of bioresorbable electronics, which provides therapeutic benefits before harmlessly dissolving like absorbable sutures, was also explored. By adjusting the composition and thickness of these devices, the team could control their functional lifespan before dissolution. The original dissolvable pacemaker worked well in pre-clinical animal studies, but cardiac surgeons suggested making the device smaller for non-invasive implantation and use in smaller patients. The device initially relied on near-field communication (NFC), the technology used in smartphones for payments and RFID tags, which required an integrated antenna. Instead of NFC for wireless control, the team created a light-based approach to turn on the pacemaker and send stimulation pulses to the heart. This innovation allowed them to drastically reduce the device's size.
Additionally, the researchers rethought the power source. Rather than using NFC, the new pacemaker operates using a galvanic cell, a simple battery that converts chemical energy into electrical energy. The pacemaker uses two different metals as electrodes that, when in contact with biofluids, form a battery. The resulting chemical reactions produce the electrical current needed to stimulate the heart. The researchers utilized an infrared light wavelength that can safely and deeply penetrate the body. If the patient’s heart rate drops below a certain threshold, the wearable device detects this and automatically activates an LED light. The light flashes on and off at a rate that matches the normal heart rate. Despite its tiny size—measuring just 1.8 millimeters in width, 3.5 millimeters in length, and 1 millimeter in thickness—the pacemaker delivers the same level of stimulation as a full-sized pacemaker. Due to its miniature size, physicians can place multiple pacemakers across the heart. By using different wavelengths of light, individual pacemakers can be independently controlled, enabling more sophisticated synchronization than traditional pacing methods. This system can pace different areas of the heart at different rhythms, potentially helping to terminate arrhythmias in special cases.
“We have developed what is, to our knowledge, the world’s smallest pacemaker,” said Northwestern bioelectronics pioneer John A. Rogers, who led the device development. “There’s a crucial need for temporary pacemakers in the context of pediatric heart surgeries, and that’s a use case where size miniaturization is incredibly important. In terms of the device load on the body — the smaller, the better.”
Latest Critical Care News
- AI Model Analyzes Patient Data to Diagnose Multiple Sclerosis With 90% Accuracy
- Magnetically Navigable Microparticles Enable Targeted Drug Delivery
- AI-Powered Algorithm Automates Analysis of Coronary Stents After Implantation
- New Stroke Risk Scoring System to Help Avoid Unnecessary Surgeries
- Wearable Device Tracks Individual Cells in Bloodstream in Real Time
- Drug Delivery System Uses Ultrasound-Activated Nanoparticles to Destroy Bacterial Biofilms
- New Potent Injectable Therapy Could Prevent Heart Failure After Heart Attack
- Hospital-Based System Combines AI and Genomic Surveillance to Quickly Detect Infectious Disease Outbreaks
- New Approach to Visualizing Blood Pressure Data Can Help Better Manage Hypertension Patients
- Breakthrough AI Technology Accurately Assesses Heart Failure Severity
- Smart Bandage Monitors Chronic Wounds in Human Patients
- AI Identifies Patients with Increased Lung Cancer Risk Up To 4 Months Earlier
- Next Gen Hemodynamic Monitoring Solution Provides AI-Driven Clinical Decision Support
- AI Algorithm Identifies High-Risk Heart Patients
- Wearable Glucose Monitor Offers Less Invasive Approach to Assessing Diabetes Risk
- Wireless, Self-Powered Smart Insole to Improve Personal Health Monitoring
Channels
Surgical Techniques
view channel
DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
One of the challenges of fighting pancreatic cancer is finding ways to penetrate the organ’s dense tissue to define the margins between malignant and normal tissue. Now, a new study uses DNA origami structures... Read more
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more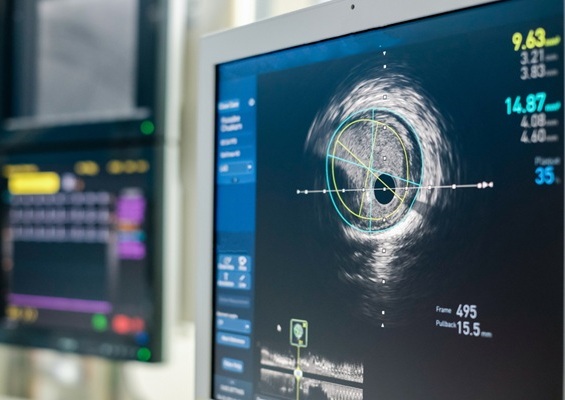
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more















