Neurorestorative Treatment Strategies Hold Promise for Most Severe Forms of Epilepsy
|
By HospiMedica International staff writers Posted on 08 Apr 2025 |
Epilepsy affects approximately 50 million people worldwide, with around 30% of these individuals, or roughly 15 million people, suffering from drug-resistant epilepsy (DRE). While some patients experience only a few seizures per month, others may have hundreds of seizures each day, ranging from mild episodes to life-threatening events. Current treatment options for DRE include surgical interventions like brain resection, where a portion of the brain tissue responsible for seizures is removed. Another approach is laser ablation therapy, which targets and destroys abnormal brain tissue using focused energy. Although these surgical methods can be effective, they carry the risk of side effects such as memory problems, motor deficits, and speech difficulties. Another surgical option, neuromodulation, uses electrical or magnetic stimulation to interrupt abnormal brain activity without removing brain tissue. However, a new and innovative trend in research is exploring the use of regenerative medicine as a "reparative" approach to help heal the brain in patients with DRE.
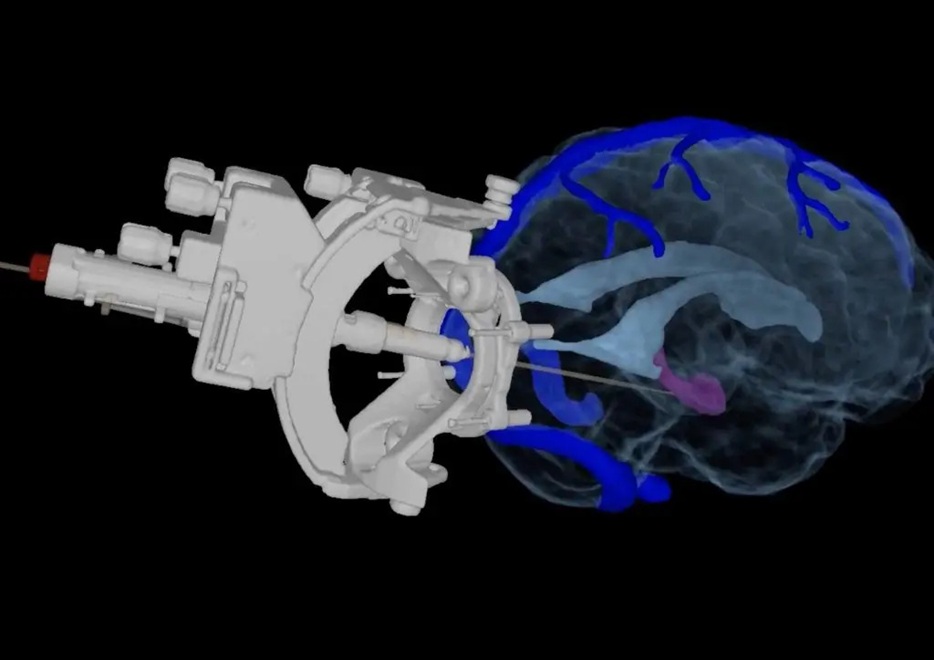
Researchers at Mayo Clinic (Rochester, MN, USA) are conducting the first-in-human clinical trial to evaluate the use of specialized inhibitory brain cells implanted as a potential reparative treatment for DRE. This minimally invasive technique involves injecting these inhibitory cells through a small, pencil eraser-sized incision at the back of the head. The goal is for these cells to integrate into the brain over time, helping to repair the neural circuitry and reducing or preventing seizures without causing the side effects associated with traditional surgical methods. Mayo Clinic's Arizona location is one of 29 sites nationwide taking part in this trial, which focuses on patients with focal epilepsy, where seizures are localized to a specific brain region.
At Mayo Clinic in Florida, another clinical trial is exploring the potential of regenerative medicine as a reparative treatment for DRE. This trial is investigating the combination of implanted stem cells and neuromodulation therapy. One of the most recent FDA-approved neuromodulation therapies for epilepsy is deep brain stimulation (DBS). While DBS has been shown to reduce seizures by up to 70% after five years, it is rare for patients to become completely seizure-free. To address this, researchers are combining DBS with stem cell therapy in hopes of enhancing the effectiveness of neuromodulation. This clinical trial involves implanting adipose-derived mesenchymal stem cells (MSCs), a type of adult stem cell with anti-inflammatory properties that may aid in healing, as an adjunct to DBS for patients with DRE.
"We've thought about this for generations, we just didn't have these technologies to enable it. Now we do," said Sanjeet Grewal, M.D., director of stereotactic and functional neurosurgery at Mayo Clinic. "So, whether it's wound healing, neurodegeneration, epilepsy or stroke, there are so many different studies going on investigating the potential of regenerative or reparative therapies."
Related Links:
Mayo Clinic
Latest Critical Care News
- AI Interpretability Tool for Photographed ECG Images Offers Pixel-Level Precision
- AI-ECG Tools Can Identify Heart Muscle Weakness in Women Before Pregnancy
- AI Model Analyzes Patient Data to Diagnose Multiple Sclerosis With 90% Accuracy
- Magnetically Navigable Microparticles Enable Targeted Drug Delivery
- AI-Powered Algorithm Automates Analysis of Coronary Stents After Implantation
- New Stroke Risk Scoring System to Help Avoid Unnecessary Surgeries
- Wearable Device Tracks Individual Cells in Bloodstream in Real Time
- Drug Delivery System Uses Ultrasound-Activated Nanoparticles to Destroy Bacterial Biofilms
- New Potent Injectable Therapy Could Prevent Heart Failure After Heart Attack
- Hospital-Based System Combines AI and Genomic Surveillance to Quickly Detect Infectious Disease Outbreaks
- New Approach to Visualizing Blood Pressure Data Can Help Better Manage Hypertension Patients
- Breakthrough AI Technology Accurately Assesses Heart Failure Severity
- Smart Bandage Monitors Chronic Wounds in Human Patients
- AI Identifies Patients with Increased Lung Cancer Risk Up To 4 Months Earlier
- Next Gen Hemodynamic Monitoring Solution Provides AI-Driven Clinical Decision Support
- AI Algorithm Identifies High-Risk Heart Patients
Channels
Surgical Techniques
view channel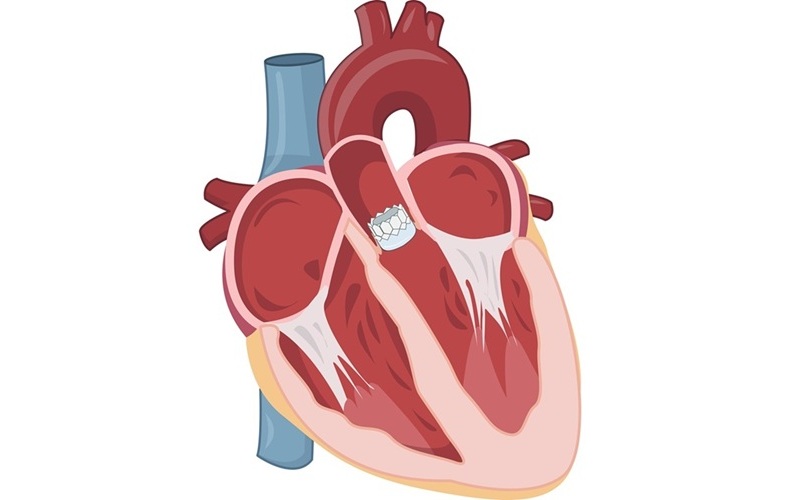
Early TAVR Intervention Reduces Cardiovascular Events in Asymptomatic Aortic Stenosis Patients
Each year, approximately 300,000 Americans are diagnosed with aortic stenosis (AS), a serious condition that results from the narrowing or blockage of the aortic valve in the heart. Two common treatments... Read more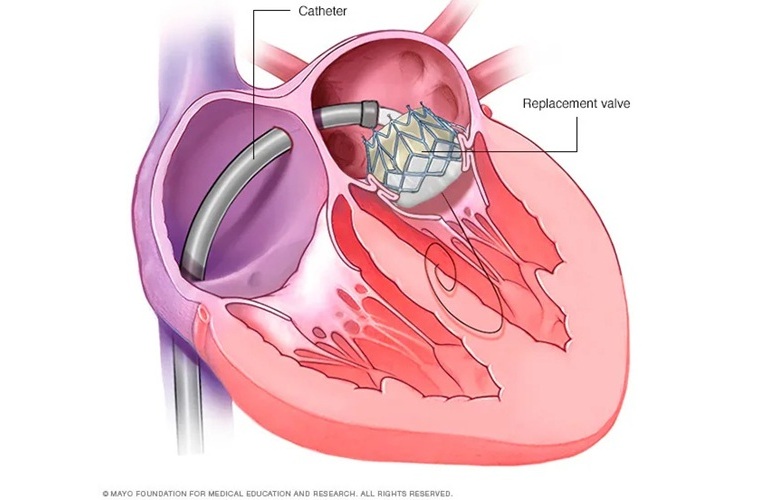
New Procedure Found Safe and Effective for Patients Undergoing Transcatheter Mitral Valve Replacement
In the United States, approximately four million people suffer from mitral valve regurgitation, the most common type of heart valve disease. As an alternative to open-heart surgery, transcatheter mitral... Read more
No-Touch Vein Harvesting Reduces Graft Failure Risk for Heart Bypass Patients
A coronary artery bypass graft (CABG) is a surgical procedure used to enhance blood flow and oxygen supply to the heart in individuals with coronary heart disease. During the procedure, a healthy blood... Read more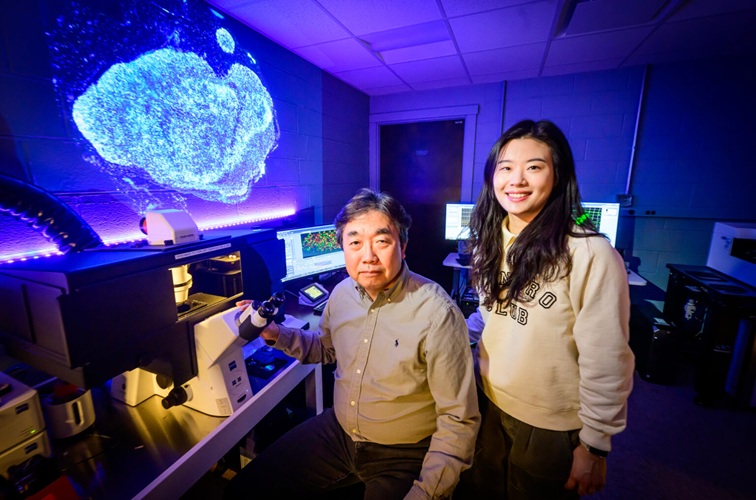
DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
One of the challenges of fighting pancreatic cancer is finding ways to penetrate the organ’s dense tissue to define the margins between malignant and normal tissue. Now, a new study uses DNA origami structures... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more














