“Black Box” Recorder Monitors Operating Rooms 
|
By HospiMedica International staff writers Posted on 29 Jul 2014 |

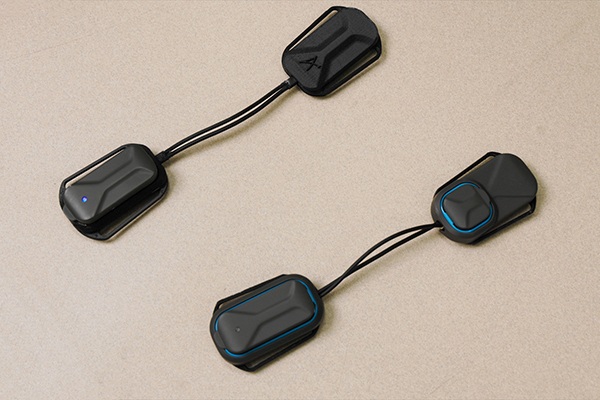
Image: The PESA Xstream “Black box” for operating rooms (Photo courtesy of PESA).
A “black box,” similar to that used in the airline industry, could improve patient safety and outcomes by identifying where errors occur in the operating room (OR) and teaching surgeons how to prevent them.
Developed at St. Michael’s Hospital (Toronto, ON, Canada), in collaboration with Air Canada (Montreal, Canada) the “black box” records almost everything that is happening in the OR, such as vital signs, a video of the OR, a video feed from the endoscope used in the surgical procedure, conversations among health care workers, room temperature, and decibel levels. Based on the PESA (Huntsville, AL, USA) X-stream multipath streaming media recorder, the technology is currently being used for minimally invasive surgery (MIS), but could be expanded for open surgeries as well.
Patients must give their consent before the black box is used during their surgery, as do members of the surgical team, including theater nurses. In a preliminary review of the data recorded on the device, the researchers have found that 84% of errors during gastric bypass MIS procedures occurred during the same two stages - suturing and grafting the bowel. The device has been in use at St. Michael’s since April 2014, and is also being tested at two hospitals in Copenhagen (Denmark), with more international sites to be involved soon.
“We want to see where errors happen in surgery so that we can understand how errors lead to adverse events and develop training curricula to prevent these errors from ever happening again,” said device developer surgeon Teodor Grantcharov, MD. “It doesn’t mean that we will have perfect surgeries, because we are not perfect. But it means we will learn from our errors, which will make us safer. We will train future surgeons better because we can show them what the most critical situations are and how to avoid them.”
“For surgeons, we will have data that will allow better coaching and improvements, and therefore better patient care. We will reduce the risk and complications and show how to make the OR more efficient, which will also allow us to save money and do more cases,” added Dr. Grantcharov. He also added that he hoped his black box would bring more transparency to the OR for patients, and help change the “blame-and-shame” culture that traditionally has made doctors and nurses reluctant to report mistakes.
Related Links:
St. Michael’s Hospital
Air Canada
PESA
Developed at St. Michael’s Hospital (Toronto, ON, Canada), in collaboration with Air Canada (Montreal, Canada) the “black box” records almost everything that is happening in the OR, such as vital signs, a video of the OR, a video feed from the endoscope used in the surgical procedure, conversations among health care workers, room temperature, and decibel levels. Based on the PESA (Huntsville, AL, USA) X-stream multipath streaming media recorder, the technology is currently being used for minimally invasive surgery (MIS), but could be expanded for open surgeries as well.
Patients must give their consent before the black box is used during their surgery, as do members of the surgical team, including theater nurses. In a preliminary review of the data recorded on the device, the researchers have found that 84% of errors during gastric bypass MIS procedures occurred during the same two stages - suturing and grafting the bowel. The device has been in use at St. Michael’s since April 2014, and is also being tested at two hospitals in Copenhagen (Denmark), with more international sites to be involved soon.
“We want to see where errors happen in surgery so that we can understand how errors lead to adverse events and develop training curricula to prevent these errors from ever happening again,” said device developer surgeon Teodor Grantcharov, MD. “It doesn’t mean that we will have perfect surgeries, because we are not perfect. But it means we will learn from our errors, which will make us safer. We will train future surgeons better because we can show them what the most critical situations are and how to avoid them.”
“For surgeons, we will have data that will allow better coaching and improvements, and therefore better patient care. We will reduce the risk and complications and show how to make the OR more efficient, which will also allow us to save money and do more cases,” added Dr. Grantcharov. He also added that he hoped his black box would bring more transparency to the OR for patients, and help change the “blame-and-shame” culture that traditionally has made doctors and nurses reluctant to report mistakes.
Related Links:
St. Michael’s Hospital
Air Canada
PESA
Latest Health IT News
- Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
- Smartwatches Could Detect Congestive Heart Failure
- Versatile Smart Patch Combines Health Monitoring and Drug Delivery
- Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
- Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
- AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
- AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
- First Fully Autonomous Generative AI Personalized Medical Authorizations System Reduces Care Delay
- Electronic Health Records May Be Key to Improving Patient Care, Study Finds
- AI Trained for Specific Vocal Biomarkers Could Accurately Predict Coronary Artery Disease
- First-Ever AI Test for Early Diagnosis of Alzheimer’s to Be Expanded to Diagnosis of Parkinson’s Disease
Channels
Artificial Intelligence
view channel
Innovative Risk Score Predicts Heart Attack or Stroke in Kidney Transplant Candidates
Heart researchers have utilized an innovative risk assessment score to accurately predict whether patients being evaluated for kidney transplants are at risk for future major cardiac events, such as a... Read more
AI Algorithm Detects Early-Stage Metabolic-Associated Steatotic Liver Disease Using EHRs
Liver disease, which is treatable when detected early, often goes unnoticed until it reaches advanced stages. Metabolic-associated steatotic liver disease (MASLD), the most prevalent form of liver disease,... Read moreCritical Care
view channel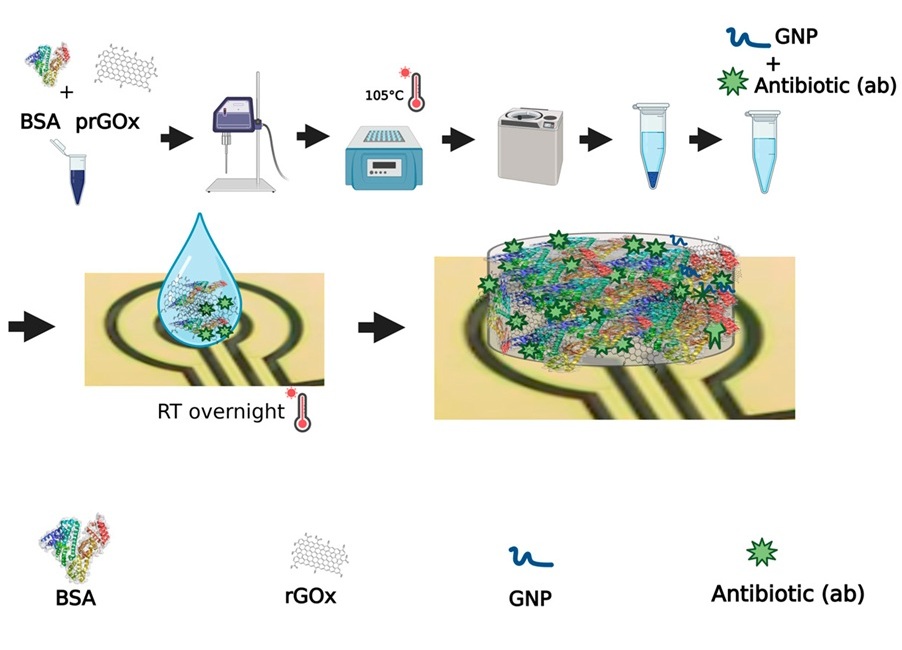
Novel Coating Significantly Extends Longevity of Implantable Biosensors
Wearable and implantable biosensors capable of accurately detecting biological molecules in a non-invasive or minimally invasive way offer enormous potential for monitoring patients’ health and their responses... Read more
Nanogel-Based Drug Delivery Technology to Improve UTI Treatment
Urinary tract infections (UTIs) are not only widespread and costly but also highly debilitating, significantly impacting the quality of life for those affected. The antibiotics commonly used to treat UTIs... Read more
New IV Pole Improves Safety and Ease of Administering IV Medications at Hospital Bedside
Preventable medication errors affect around 500,000 hospitalized patients in the U.S. every year. A significant portion of these errors occur with intravenous (IV) smart pumps, which require a precise... Read moreSurgical Techniques
view channel
Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
Surgical adhesions are a frequent and often life-threatening complication following open or laparoscopic abdominal surgery. These adhesions develop in the weeks following surgery as the body heals.... Read more
Groundbreaking Leadless Pacemaker to Prevent Invasive Surgeries for Children
Leadless pacemakers marked a significant advancement in cardiac care, primarily because traditional pacemakers are dependent on leads, which are prone to breakage over time. Currently, two FDA-approved... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read morePoint of Care
view channel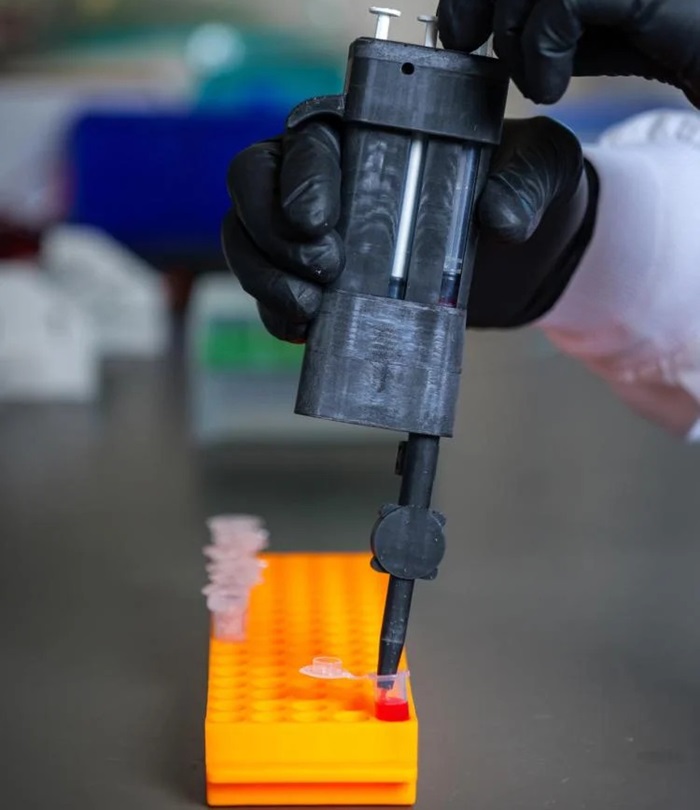
Handheld, Sound-Based Diagnostic System Delivers Bedside Blood Test Results in An Hour
Patients who go to a doctor for a blood test often have to contend with a needle and syringe, followed by a long wait—sometimes hours or even days—for lab results. Scientists have been working hard to... Read more
Smartphone-Enabled, Paper-Based Quantitative Diagnostic Platform Transforms POC Testing
Point-of-care diagnostics are crucial for public health, offering rapid, on-site testing that enables prompt diagnosis and treatment. This is especially valuable in remote or underserved regions where... Read moreBusiness
view channel
Becton Dickinson to Spin Out Biosciences and Diagnostic Solutions Business
Becton, Dickinson and Company (BD, Franklin Lakes, NJ, USA), has announced that its board of directors has unanimously authorized BD management to pursue a plan to separate BD's Biosciences and Diagnostic... Read more