3D-Printing Technique Fabricates Microphysiological Devices
|
By HospiMedica International staff writers Posted on 09 Nov 2016 |
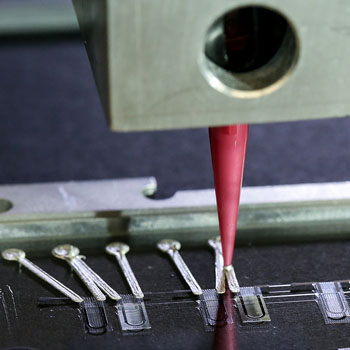
Image: Close up of 3D printer printing heart-on-a-chip MPD (Photo courtesy of Harvard University).
Multi-material three-dimensional (3D) printing may one day be used to design organs-on-chips that match the properties of a specific disease, or even an individual patient’s cells.
Researchers at Harvard University (Cambridge, MA, USA) have developed a new technique to fabricate instrumented cardiac microphysiological devices (MPDs) that uses a mix of six functional inks that are based on piezo-resistive, high-conductance, biocompatible soft materials. By using 3D printing, the researchers were able to print a physio-mimetic, laminar cardiac tissue MPD that integrates soft strain sensors into the micro-architecture of the tissue, all in a single, continuous procedure.
The chip contains multiple wells, each with separate tissues and integrated sensors, which allows the researchers to study many engineered cardiac tissues at once. To demonstrate the efficacy of the device, the researchers first validated that the embedded sensors provided non-invasive, electronic readouts of tissue contractile stresses inside cell incubator environments. They then used the MPD to study drug responses, as well as the contractile development of human stem cell-derived laminar cardiac tissues over four weeks. The study was published on October 24, 2016, in Nature Materials.
“Researchers are often left working in the dark when it comes to gradual changes that occur during cardiac tissue development and maturation, because there has been a lack of easy, non-invasive ways to measure the tissue functional performance,” said lead author Johan Ulrik Lind, PhD. “These integrated sensors allow researchers to continuously collect data while tissues mature and improve their contractility. Similarly, they will enable studies of gradual effects of chronic exposure to toxins.”
“Our microfabrication approach opens new avenues for in vitro tissue engineering, toxicology, and drug screening research,” said study co-author professor of bioengineering and applied physics Kit Parker, PhD. “Translating microphysiological devices into truly valuable platforms for studying human health and disease requires that we address both data acquisition and manufacturing of our devices. This work offers new potential solutions to both of these central challenges.”
MPDs, also known as organs-on-chips, mimic the structure and function of native tissue in-vitro and have emerged as a promising alternative to traditional animal testing; but the fabrication and data collection process is expensive and laborious. Currently, these devices are built in clean rooms using a complex, multi-step lithographic process, and collecting data requires microscopy or high-speed cameras, since they do not have integrated sensors.
Related Links:
Harvard University
Researchers at Harvard University (Cambridge, MA, USA) have developed a new technique to fabricate instrumented cardiac microphysiological devices (MPDs) that uses a mix of six functional inks that are based on piezo-resistive, high-conductance, biocompatible soft materials. By using 3D printing, the researchers were able to print a physio-mimetic, laminar cardiac tissue MPD that integrates soft strain sensors into the micro-architecture of the tissue, all in a single, continuous procedure.
The chip contains multiple wells, each with separate tissues and integrated sensors, which allows the researchers to study many engineered cardiac tissues at once. To demonstrate the efficacy of the device, the researchers first validated that the embedded sensors provided non-invasive, electronic readouts of tissue contractile stresses inside cell incubator environments. They then used the MPD to study drug responses, as well as the contractile development of human stem cell-derived laminar cardiac tissues over four weeks. The study was published on October 24, 2016, in Nature Materials.
“Researchers are often left working in the dark when it comes to gradual changes that occur during cardiac tissue development and maturation, because there has been a lack of easy, non-invasive ways to measure the tissue functional performance,” said lead author Johan Ulrik Lind, PhD. “These integrated sensors allow researchers to continuously collect data while tissues mature and improve their contractility. Similarly, they will enable studies of gradual effects of chronic exposure to toxins.”
“Our microfabrication approach opens new avenues for in vitro tissue engineering, toxicology, and drug screening research,” said study co-author professor of bioengineering and applied physics Kit Parker, PhD. “Translating microphysiological devices into truly valuable platforms for studying human health and disease requires that we address both data acquisition and manufacturing of our devices. This work offers new potential solutions to both of these central challenges.”
MPDs, also known as organs-on-chips, mimic the structure and function of native tissue in-vitro and have emerged as a promising alternative to traditional animal testing; but the fabrication and data collection process is expensive and laborious. Currently, these devices are built in clean rooms using a complex, multi-step lithographic process, and collecting data requires microscopy or high-speed cameras, since they do not have integrated sensors.
Related Links:
Harvard University
Latest Health IT News
- Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
- Smartwatches Could Detect Congestive Heart Failure
- Versatile Smart Patch Combines Health Monitoring and Drug Delivery
- Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
- Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
- AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
- AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
- First Fully Autonomous Generative AI Personalized Medical Authorizations System Reduces Care Delay
- Electronic Health Records May Be Key to Improving Patient Care, Study Finds
- AI Trained for Specific Vocal Biomarkers Could Accurately Predict Coronary Artery Disease
Channels
Critical Care
view channel
Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
Intestinal gases are associated with several health conditions, including colon cancer, irritable bowel syndrome, and inflammatory bowel disease, and they have the potential to serve as crucial biomarkers... Read moreNovel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
Multiphoton microscopy has become an invaluable tool in neuroscience, allowing researchers to observe brain activity in real time with high-resolution imaging. A crucial aspect of many multiphoton microscopy... Read more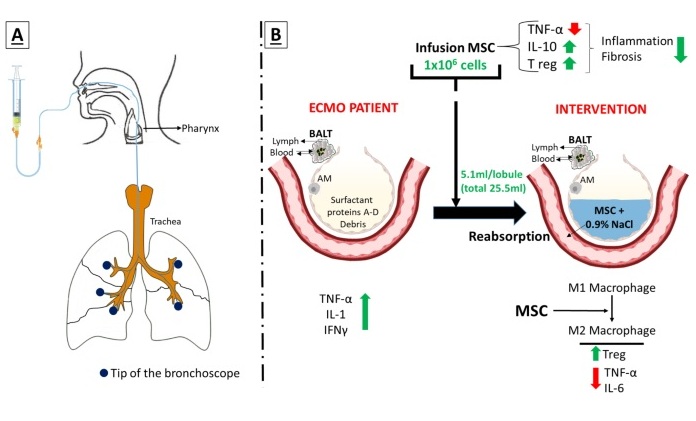
Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
Until now, administering cell therapies to patients on extracorporeal membrane oxygenation (ECMO)—a life-support system typically used for severe lung failure—has been nearly impossible.... Read moreSurgical Techniques
view channel
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more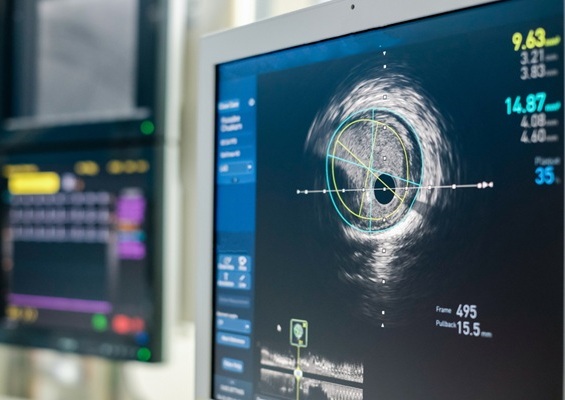
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more