Experimental Drug Blocks SARS-CoV-2 from Entering Lung Cells
|
By HospiMedica International staff writers Posted on 21 Sep 2020 |

Illustration
In a new study, an experimental compound has prevented the SARS-CoV-2 virus that causes COVID-19 from entering human airway cells.
Researchers at the NYU Grossman School of Medicine (New York City, NY) have been focusing their research on the structure of SARS-CoV-2. The virus has on its surface a spike protein that can attach to angiotensin converting enzyme 2 (ACE2), a protein on the surface of cells lining human lungs. Once attached, the spike pulls the virus close to a cell, which lets it fuse to it and enter it, and then hijack the cell's machinery to make copies of itself. For this reason, molecular biologists have sought to engineer forms of ACE2 that, instead of being woven onto the cell surface, float freely. They hope that free-floating ACE2 could serve as a decoy that competes with the membrane-bound counterpart for the viral spike protein, thereby blocking the virus’ entry.
In a new investigative effort, the researchers made key changes to a free ACE2 molecule, and then fused one part of it to a piece of an antibody, an immune system protein, with the goal of strengthening its antiviral effect. The team calls their molecule an "ACE-2 microbody." To build the microbody, the team used a standard technique in molecular biology, which creates a "fusion protein" by building a DNA molecule in which two genes, each with instructions for a different protein, are linked. The linked genes are then introduced into a mammalian cell, which makes the hybrid protein from the hybrid instructions.
For the current work, the researchers started with the ectodomain of ACE2, the part of the protein that sticks out from a cell's surface and attaches to the viral spike protein. They changed the ectodomain's genetic code to swap out one amino acid building block, replacing a histidine at position 345 in the protein's structure with an alanine. The modification kept ACE-2 from interacting with angiotensin, a hormone that regulates blood pressure, its natural role and a possible source of side effects. For the second piece of their fusion compound, the researchers used an Fc domain, the part of an antibody's structure that turns on other parts of the immune system when the antibody encounters an invading microbe. The team intentionally shortened the domain, however, to prevent off-target immune effects.
The researchers wanted the Fc domain on the microbody because such proteins form strong disulfide bonds when they encounter one other. The binding of two fusion proteins through their Fc domains creates a dimer, a stable structure that attaches more strongly to the virus because it now has two ACE2 ectodomains to cling to viral spikes, according to the researchers. To determine how strongly their experimental drug could interact with the COVID-19 virus, the research team used a "pseudotyped" virus, a vital tool used in decades of HIV research. To make it, the researchers started with HIV viruses, but removed the disease-causing part of their genetic material to make them safe to work with. To these engineered viral particles the team then added the SARS-CoV-2 spike protein, as well as a gene encoding the firefly protein luciferase.
Like the current coronavirus, the pseudotyped virus could infect cells by using the SARS-CoV-2 spike to attach to ACE-2. With the firefly gene included, cells infected by the test virus glowed, and glowed brighter the more viral particles they were infected with. By mixing the ACE-2 microbody with the pseudotyped virus, infecting cells and then measuring the glow, the researchers could tell how well their new molecule blocked viral entry. The researchers have cautioned that any signals of effectiveness for the experimental drug would need to be confirmed in animal studies, and then in human trials if appropriate.
"In our tests, the ACE-2 microbody was about ten times as effective at blocking virus entry as unmodified forms of ACE2 studied previously," said corresponding study author Nathaniel Landau, PhD, professor in the Department of Microbiology at NYU Langone Health. "We call our compound a microbody because, by using just the key parts of each protein, the drug molecule is smaller and potentially easier to make than versions made up of complete proteins."
"An advantage of the study drug is that, by competing for the spike with the ACE2 membrane-bound receptor, infection is blocked before it can start," said first study author Takuya Tada, PhD, a post-doctoral scholar in Landau's lab. "Coronaviruses are quick to evolve around treatments, like therapeutic antibodies, that target one structural feature on the virus, but will have a harder time changing the entire first step by which they enter cells."
Related Links:
NYU Grossman School of Medicine
Researchers at the NYU Grossman School of Medicine (New York City, NY) have been focusing their research on the structure of SARS-CoV-2. The virus has on its surface a spike protein that can attach to angiotensin converting enzyme 2 (ACE2), a protein on the surface of cells lining human lungs. Once attached, the spike pulls the virus close to a cell, which lets it fuse to it and enter it, and then hijack the cell's machinery to make copies of itself. For this reason, molecular biologists have sought to engineer forms of ACE2 that, instead of being woven onto the cell surface, float freely. They hope that free-floating ACE2 could serve as a decoy that competes with the membrane-bound counterpart for the viral spike protein, thereby blocking the virus’ entry.
In a new investigative effort, the researchers made key changes to a free ACE2 molecule, and then fused one part of it to a piece of an antibody, an immune system protein, with the goal of strengthening its antiviral effect. The team calls their molecule an "ACE-2 microbody." To build the microbody, the team used a standard technique in molecular biology, which creates a "fusion protein" by building a DNA molecule in which two genes, each with instructions for a different protein, are linked. The linked genes are then introduced into a mammalian cell, which makes the hybrid protein from the hybrid instructions.
For the current work, the researchers started with the ectodomain of ACE2, the part of the protein that sticks out from a cell's surface and attaches to the viral spike protein. They changed the ectodomain's genetic code to swap out one amino acid building block, replacing a histidine at position 345 in the protein's structure with an alanine. The modification kept ACE-2 from interacting with angiotensin, a hormone that regulates blood pressure, its natural role and a possible source of side effects. For the second piece of their fusion compound, the researchers used an Fc domain, the part of an antibody's structure that turns on other parts of the immune system when the antibody encounters an invading microbe. The team intentionally shortened the domain, however, to prevent off-target immune effects.
The researchers wanted the Fc domain on the microbody because such proteins form strong disulfide bonds when they encounter one other. The binding of two fusion proteins through their Fc domains creates a dimer, a stable structure that attaches more strongly to the virus because it now has two ACE2 ectodomains to cling to viral spikes, according to the researchers. To determine how strongly their experimental drug could interact with the COVID-19 virus, the research team used a "pseudotyped" virus, a vital tool used in decades of HIV research. To make it, the researchers started with HIV viruses, but removed the disease-causing part of their genetic material to make them safe to work with. To these engineered viral particles the team then added the SARS-CoV-2 spike protein, as well as a gene encoding the firefly protein luciferase.
Like the current coronavirus, the pseudotyped virus could infect cells by using the SARS-CoV-2 spike to attach to ACE-2. With the firefly gene included, cells infected by the test virus glowed, and glowed brighter the more viral particles they were infected with. By mixing the ACE-2 microbody with the pseudotyped virus, infecting cells and then measuring the glow, the researchers could tell how well their new molecule blocked viral entry. The researchers have cautioned that any signals of effectiveness for the experimental drug would need to be confirmed in animal studies, and then in human trials if appropriate.
"In our tests, the ACE-2 microbody was about ten times as effective at blocking virus entry as unmodified forms of ACE2 studied previously," said corresponding study author Nathaniel Landau, PhD, professor in the Department of Microbiology at NYU Langone Health. "We call our compound a microbody because, by using just the key parts of each protein, the drug molecule is smaller and potentially easier to make than versions made up of complete proteins."
"An advantage of the study drug is that, by competing for the spike with the ACE2 membrane-bound receptor, infection is blocked before it can start," said first study author Takuya Tada, PhD, a post-doctoral scholar in Landau's lab. "Coronaviruses are quick to evolve around treatments, like therapeutic antibodies, that target one structural feature on the virus, but will have a harder time changing the entire first step by which they enter cells."
Related Links:
NYU Grossman School of Medicine
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read more
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read moreSurgical Techniques
view channel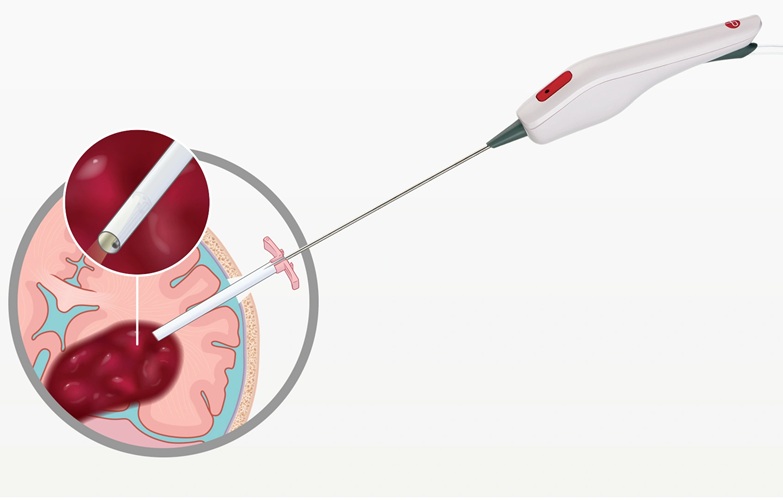
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read more
Novel Glue Prevents Complications After Breast Cancer Surgery
Seroma and prolonged lymphorrhea are among the most common complications following axillary lymphadenectomy in breast cancer patients. These postoperative issues can delay recovery and postpone the start... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more