First-Ever COVID-19 Severity Test to Triage Patients Quickly and Accurately
|
By HospiMedica International staff writers Posted on 27 Nov 2020 |

Image: AbioSCOPE (Photo courtesy of Abionic SA)
A new test offers medical criteria of COVID-19 severity and likelihood of clinical deterioration within minutes of analyzing a blood sample, allowing healthcare practitioners to decide whether COVID-19 patients should be assigned to general wards, intensive care units (ICUs) or be discharged from the hospital.
Abionic SA (Lausanne, Switzerland) has developed the cSOFA score (Covid Sequential Organ Failure Assessment), the first-ever test that measures the likelihood of clinical deterioration in COVID-19 patients, enabling triage and assignment to the general ward or ICU upon admission and during the patients’ hospital stay. A low score allows medical decisions to be made on safely discharging patients from the hospital or moving them from the ICU to the general ward, freeing up much-needed ICU and hospital capacities.
The cSOFA score is a further development from the already widespread SOFA1 score. The two scores correlate very well, although the cSOFA score is obtained much more quickly, taking only five minutes. Due to its speed, it can serve as a monitoring parameter during hospital stays in order to identify deterioration in COVID-19 patients before the presence of clear clinical signs. Using the cSOFA score, healthcare practitioners can make an informed decision on where and how to treat patients.
In order to obtain the cSOFA score, a 30 ul drop of capillary blood is sufficient. The blood sampling can be done already upon admission by a receptionist; medical training is not necessary. Within five minutes, a score is determined that serves as a base for a decision on assigning COVID-19 patients to general wards, ICUs or allowing them to recover at home. As a result of this triage, capacities in hospitals are protected and patients receive appropriate care.
The score has obtained the authorization to sell in Europe (CE mark) and relies on PSP (pancreatic stone protein), a novel biomarker that has already been clinically validated and marketed by Abionic. PSP is characterized by its diagnostic accuracy in predicting sepsis and/or multiple organ dysfunction in various types of critically ill patients. Data from 150+ COVID-19 patients from the first European wave of SARS-CoV-2 infections showed a strong link between PSP concentration and the degradation of these patients.
“COVID-19 patients may have an adverse clinical course that is not predictive and may require emergency management with transfers to intermediate and intensive care,” said Dr. François Ventura from the University Hospital of Geneva (HUG). “The cSOFA is a great tool to help predict these possible clinical deteriorations and to guide patients through the healthcare system, which is certainly very useful in these times of healthcare system overload.”
“Measuring COVID-19 severity and likelihood of clinical deterioration protects hospitals around the globe from preventable overload and makes sure patients are treated according to their needs,” said Dr. Nicolas Durand, CEO of Abionic. “Our research also indicates that modifications to the cSOFA score may be used as severity measures for other illnesses, such as flu, sepsis and other inflammatory disorders.”
Related Links:
Abionic SA
Abionic SA (Lausanne, Switzerland) has developed the cSOFA score (Covid Sequential Organ Failure Assessment), the first-ever test that measures the likelihood of clinical deterioration in COVID-19 patients, enabling triage and assignment to the general ward or ICU upon admission and during the patients’ hospital stay. A low score allows medical decisions to be made on safely discharging patients from the hospital or moving them from the ICU to the general ward, freeing up much-needed ICU and hospital capacities.
The cSOFA score is a further development from the already widespread SOFA1 score. The two scores correlate very well, although the cSOFA score is obtained much more quickly, taking only five minutes. Due to its speed, it can serve as a monitoring parameter during hospital stays in order to identify deterioration in COVID-19 patients before the presence of clear clinical signs. Using the cSOFA score, healthcare practitioners can make an informed decision on where and how to treat patients.
In order to obtain the cSOFA score, a 30 ul drop of capillary blood is sufficient. The blood sampling can be done already upon admission by a receptionist; medical training is not necessary. Within five minutes, a score is determined that serves as a base for a decision on assigning COVID-19 patients to general wards, ICUs or allowing them to recover at home. As a result of this triage, capacities in hospitals are protected and patients receive appropriate care.
The score has obtained the authorization to sell in Europe (CE mark) and relies on PSP (pancreatic stone protein), a novel biomarker that has already been clinically validated and marketed by Abionic. PSP is characterized by its diagnostic accuracy in predicting sepsis and/or multiple organ dysfunction in various types of critically ill patients. Data from 150+ COVID-19 patients from the first European wave of SARS-CoV-2 infections showed a strong link between PSP concentration and the degradation of these patients.
“COVID-19 patients may have an adverse clinical course that is not predictive and may require emergency management with transfers to intermediate and intensive care,” said Dr. François Ventura from the University Hospital of Geneva (HUG). “The cSOFA is a great tool to help predict these possible clinical deteriorations and to guide patients through the healthcare system, which is certainly very useful in these times of healthcare system overload.”
“Measuring COVID-19 severity and likelihood of clinical deterioration protects hospitals around the globe from preventable overload and makes sure patients are treated according to their needs,” said Dr. Nicolas Durand, CEO of Abionic. “Our research also indicates that modifications to the cSOFA score may be used as severity measures for other illnesses, such as flu, sepsis and other inflammatory disorders.”
Related Links:
Abionic SA
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Artificial Intelligence
view channelCritical Care
view channel
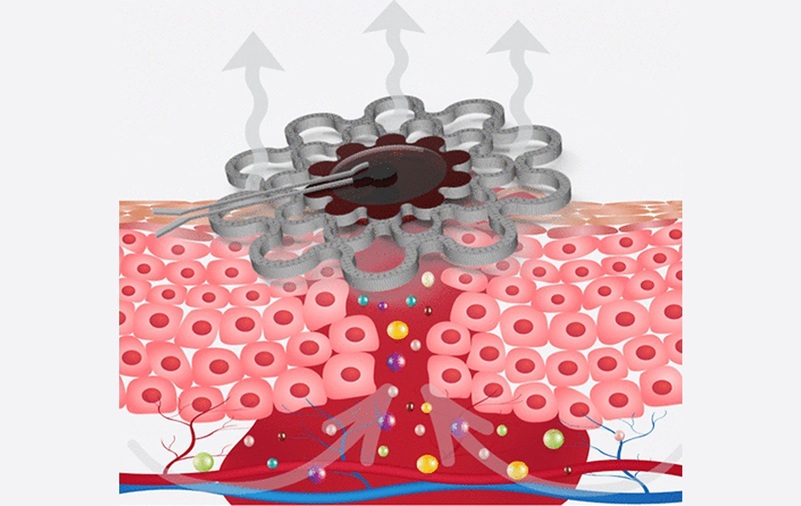
Painless Microneedle Skin Patch Monitors Immune Health
Studying immune responses typically requires blood draws or skin biopsies, both of which are invasive and sometimes uncomfortable. Many critical immune cells reside in tissues such as the skin, making... Read more
Smart T-Shirt Uses AI to Enhance Detection of Heart Rhythm Disorders
Inherited heart rhythm disorders are often missed because arrhythmias may not occur during brief testing or can appear normal on routine scans, allowing risk to go undetected. As a result, delayed diagnosis... Read moreSurgical Techniques
view channel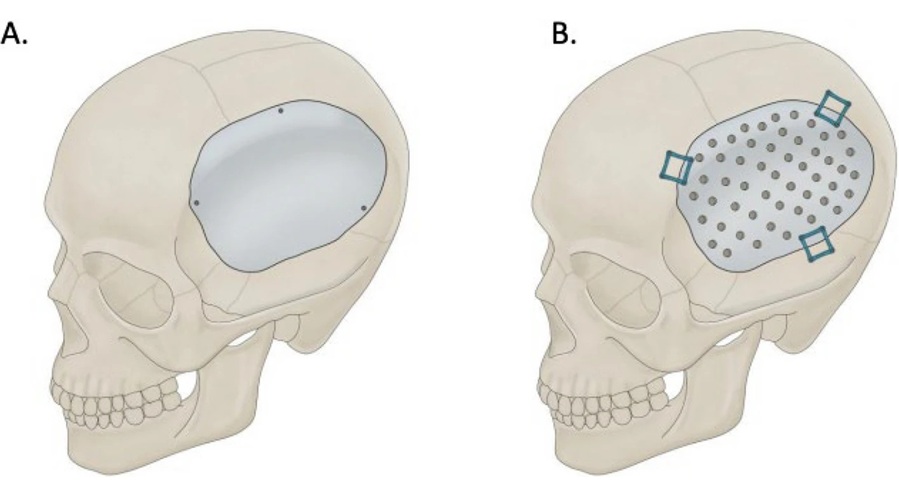
Skull Implant Design Could Shape Surgical Outcomes
Cranioplasty is a common neurosurgical procedure performed to repair skull defects after decompressive craniectomy. In addition to restoring protection to the brain, the surgery can enhance neurological... Read more
Redesigned Surgical Laser Cuts Bone Deeper and Faster Than Before
Lasers are valued in surgery for their precision and non-contact cutting, reducing mechanical stress and minimizing microcracks. While widely used for soft tissue, their application in hard tissues such... Read more
Laser Ablation Plus Immunotherapy Improves Survival in Recurrent Glioblastoma
Recurrent high-grade astrocytoma, including glioblastoma, is difficult to treat and often returns after surgery. Patients with recurrence typically survive only four to five months, highlighting a critical... Read more
New Method Offers Less Invasive Detection of Susceptibility to Rare Anesthesia Reaction
Malignant hyperthermia (MH) is a rare, inherited reaction to general anesthetics that can be rapidly fatal without prompt recognition and treatment. Definitive preoperative testing today relies on an open... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
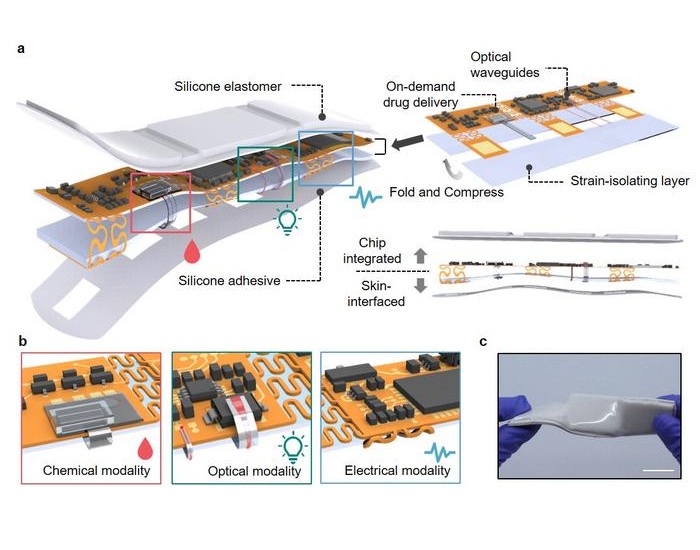
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more