AI More Accurate than Sonographers in Assessing and Diagnosing Cardiac Function
|
By HospiMedica International staff writers Posted on 03 Sep 2022 |
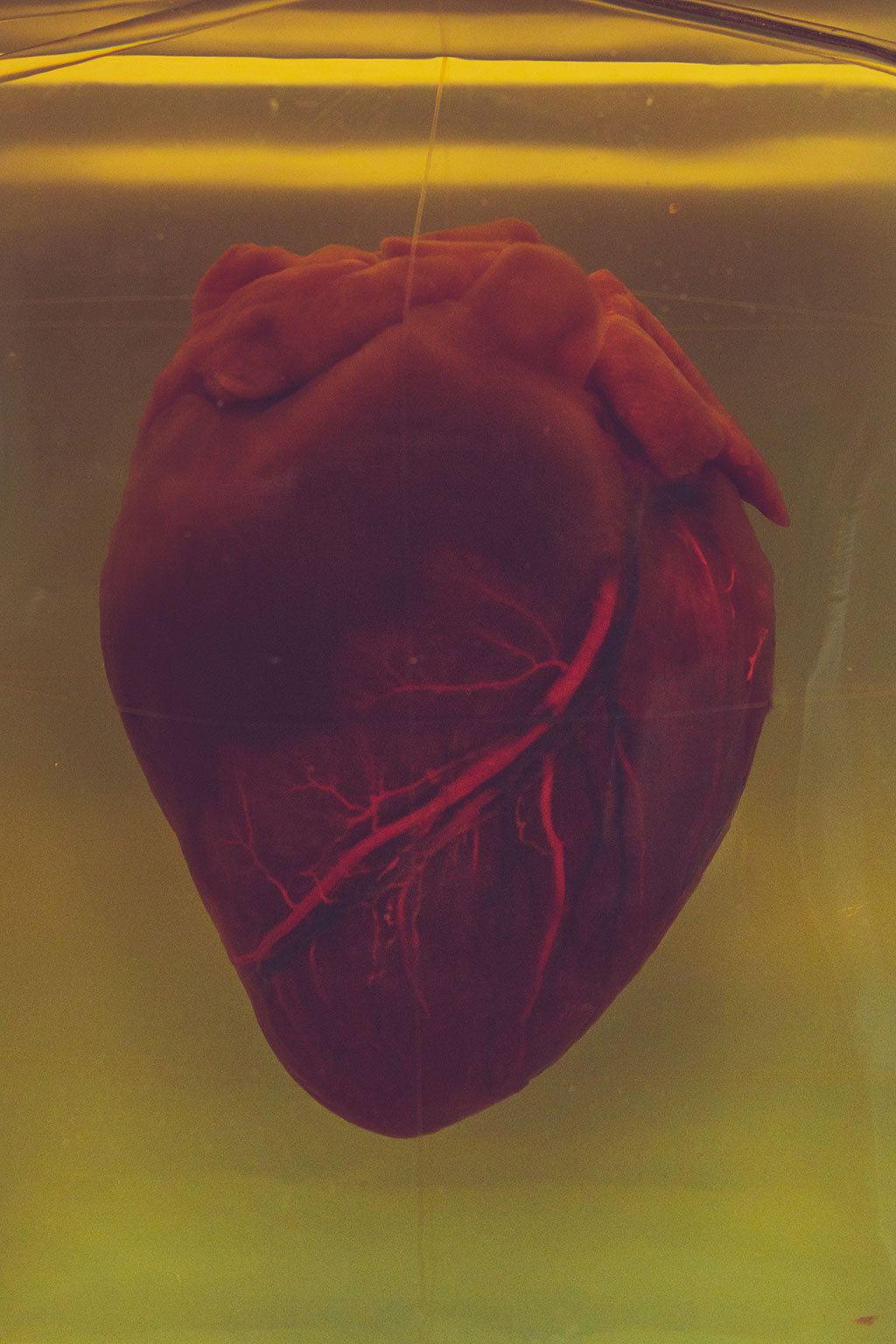
Accurate assessment of left ventricular ejection fraction (LVEF) is essential for diagnosing cardiovascular disease and making treatment decisions. However, human assessment is often based on a small number of cardiac cycles that can result in high inter-observer variability. Now, a new study has found that preliminary assessment by artificial intelligence (AI) is superior to initial sonographer assessment in patients undergoing echocardiographic evaluation of cardiac function.
EchoNet-Dynamic is a deep learning algorithm that was trained on echocardiogram videos to assess cardiac function and was previously shown to assess LVEF with a mean absolute error of 4.1-6.0%. The algorithm uses information across multiple cardiac cycles to minimize error and produce consistent results. Researchers at the Smidt Heart Institute at Cedars-Sinai (Los Angeles, CA, USA) tested whether AI or sonographer assessment of LVEF is more frequently adjusted by a reviewing cardiologist. The standard clinical workflow for determining LVEF by echocardiography is that a sonographer scans the patient; the sonographer provides an initial assessment of LVEF; and then a cardiologist reviews the assessment to provide a final report of LVEF. In this clinical trial, the sonographer’s scan was randomly allocated 1:1 to AI initial assessment or sonographer initial assessment, after which blinded cardiologists reviewed the assessment and provided a final report of LVEF.
The researchers compared how much cardiologists changed the initial assessment by AI to how much they changed the initial assessment by sonographer. The primary endpoint was the frequency of a greater than 5% change in LVEF between the initial assessment (AI or sonographer) and the final cardiologist report. The trial was designed to test for non-inferiority, with a secondary objective of testing for superiority. The study included 3,495 transthoracic echocardiograms performed on adults for any clinical indication. The proportion of studies substantially changed was 16.8% in the AI group and 27.2% in the sonographer group (difference -10.4%, 95% confidence interval [CI] -13.2% to -7.7%, p<0.001 for non-inferiority, p<0.001 for superiority). The safety endpoint was the difference between the final cardiologist report and a historical cardiologist report. The mean absolute difference was 6.29% in the AI group and 7.23% in the sonographer group (difference -0.96%, 95% CI -1.34% to -0.54%, p<0.001 for superiority).
“There has been much excitement about the use of AI in medicine, but the technologies are rarely assessed in prospective clinical trials,” said Dr. David Ouyang of the Smidt Heart Institute at Cedars-Sinai. “We previously developed one of the first AI technologies to assess cardiac function (left ventricular ejection fraction; LVEF) in echocardiograms and in this blinded, randomized trial, we compared it head to head with sonographer tracings. This trial was powered to show non-inferiority of the AI compared to sonographer tracings, and so we were pleasantly surprised when the results actually showed superiority with respect to the pre-specified outcomes.”
“We learned a lot from running a randomized trial of an AI algorithm, which hasn’t been done before in cardiology,” added Dr. Ouyang. “First, we learned that this type of trial is highly feasible in the right setting, where the AI algorithm can be integrated into the usual clinical workflow in a blinded fashion. Second, we learned that blinding really can work well in this situation. We asked our cardiologist over-readers to guess if they thought the tracing they had just reviewed was performed by AI or by a sonographer, and it turns out that they couldn’t tell the difference – which both speaks to the strong performance of the AI algorithm as well as the seamless integration into clinical software. We believe these are all good signs for future trial research in the field.”
“We are excited by the implications of the trial. What this means for the future is that certain AI algorithms, if developed and integrated in the right way, could be very effective at not only improving the quality of echo reading output but also increasing efficiencies in time and effort spent by sonographers and cardiologists by simplifying otherwise tedious but important tasks,” concluded Dr. Ouyang. “Embedding AI into clinical workflows could potentially provide more precise and consistent evaluations, thereby enabling earlier detection of clinical deterioration or response to treatment.”
Related Links:
Cedars-Sinai
Latest Critical Care News
- AI Doubles Medical Professionals’ Accuracy in Reading EEG Charts of ICU Patients
- Flexible Device Enables Sweat Gland Stimulation and Simultaneous Biosensing
- WHO Publishes First Global Guidelines to Reduce Bloodstream Infections from Catheter Use
- Innovative Material Paves Way for Next-Generation Wearable Devices
- Wireless Electronic Suture Enables Postoperative Long-Term Monitoring Of Soft Tissue
- Transcatheter Valve Replacement Outcomes Similar To Surgery, Finds Study
- Revascularization Improves Life Quality in Chronic Limb-Threatening Ischemia, Finds Study
- Powerful AI Risk Assessment Tool Predicts Outcomes in Heart Failure Patients
- Peptide-Based Hydrogels Repair Damaged Organs and Tissues On-The-Spot
- One-Hour Endoscopic Procedure Could Eliminate Need for Insulin for Type 2 Diabetes
- AI Can Prioritize Emergency Department Patients Requiring Urgent Treatment
- AI to Improve Diagnosis of Atrial Fibrillation
- Stretchable Microneedles to Help In Accurate Tracking of Abnormalities and Identifying Rapid Treatment
- Machine Learning Tool Identifies Rare, Undiagnosed Immune Disorders from Patient EHRs
- On-Skin Wearable Bioelectronic Device Paves Way for Intelligent Implants
- First-Of-Its-Kind Dissolvable Stent to Improve Outcomes for Patients with Severe PAD
Channels
Critical Care
view channel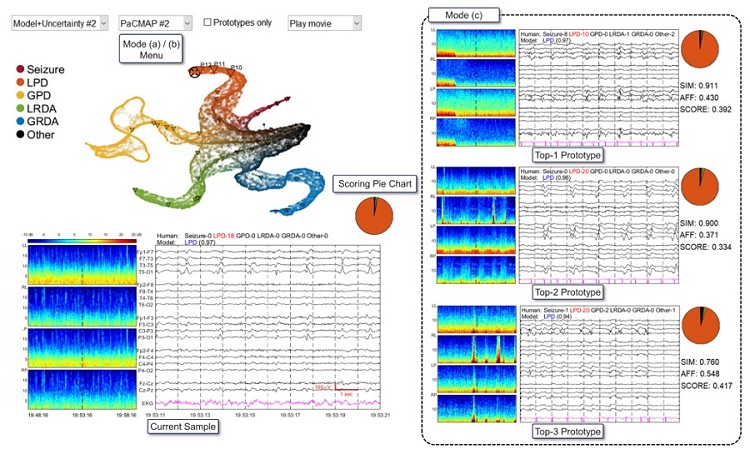
AI Doubles Medical Professionals’ Accuracy in Reading EEG Charts of ICU Patients
Electroencephalography (EEG) readings are crucial for detecting when unconscious patients may be experiencing or are at risk of seizures. EEGs involve placing small sensors on the scalp to measure the... Read moreFlexible Device Enables Sweat Gland Stimulation and Simultaneous Biosensing
Human sweat is rich in biomarkers that can be used to monitor a range of health conditions, from diabetes to genetic disorders. Many users prefer sweat sampling over blood collection because it is painless.... Read more
WHO Publishes First Global Guidelines to Reduce Bloodstream Infections from Catheter Use
Up to 70% of all inpatients require a catheter, specifically a peripherally inserted catheter (PIVC), at some point during their hospital stay. Patients who receive treatments via catheters are particularly... Read moreSurgical Techniques
view channel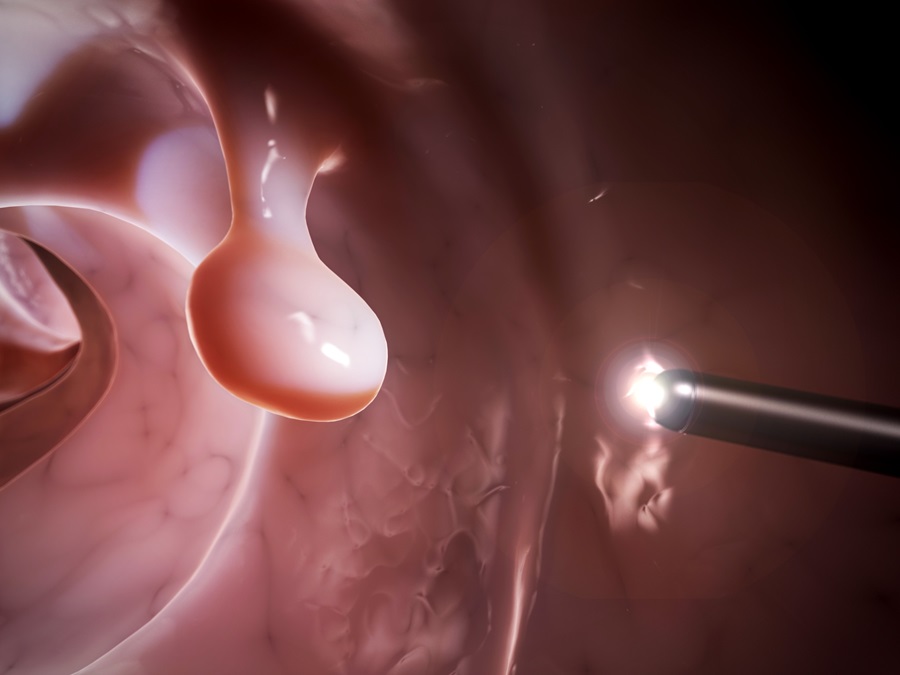
Study Warns Against Dangerous Smoke Levels Produced During Endoscopic Gastrointestinal Procedures
Healthcare professionals involved in certain smoke-generating endoscopic gastrointestinal procedures, such as those using electrical current to excise polyps, may be exposed to toxin levels comparable... Read more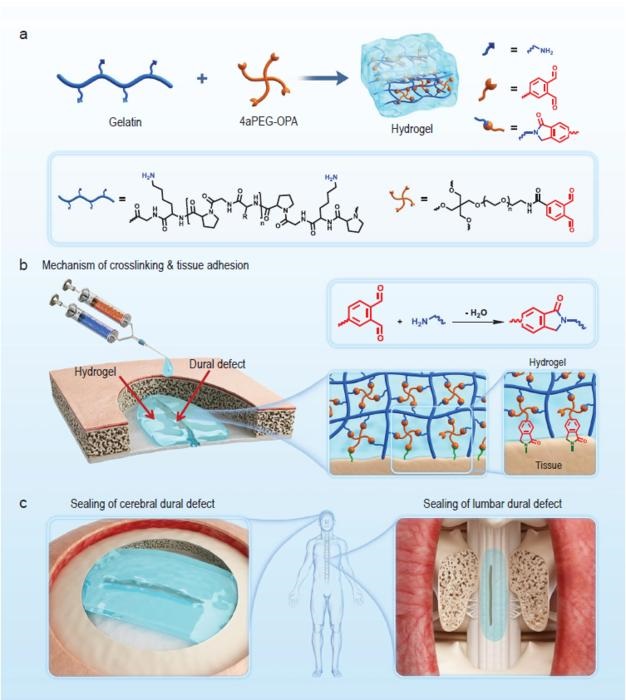
New Hydrogel Sealant Effective at Sealing Dural Defects and Preventing Postoperative Adhesion
The dura mater is a fibrous membrane of connective tissue that envelops the brain and spinal cord. In neurosurgical procedures that require access to the brain or spinal cord, opening the dura mater often... Read more
MRI-Guided Multi-Stage Robotic Positioner Enhances Stereotactic Neurosurgery Precision
Magnetic resonance imaging (MRI) offers significant benefits in neurosurgery, providing detailed 3D visualizations of neurovascular structures and tumors. Traditionally, its use has been restricted to... Read morePatient Care
view channelFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel
POCT for Infectious Diseases Delivers Laboratory Equivalent Pathology Results
On-site pathology tests for infectious diseases in rural and remote locations can achieve the same level of reliability and accuracy as those conducted in hospital laboratories, a recent study suggests.... Read more
Cartridge-Based Hemostasis Analyzer System Enables Faster Coagulation Testing
Quickly assessing a patient's total hemostasis status can be critical to influencing clinical outcomes and using blood products. Haemonetics Corporation (Boston, MA, USA) has now obtained 510(k) clearance... Read more
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read moreBusiness
view channel
MEDICA INNOVATION FORUM for the Healthcare Innovations of the Future
By always offering innovations and updating existing program formats, the internationally leading medical trade fair MEDICA in Düsseldorf has been successful for over half a century and always gives its... Read more
















