New Immunosensor Paves Way to Rapid POC Testing for COVID-19 and Emerging Infectious Diseases
|
By HospiMedica International staff writers Posted on 19 Dec 2022 |
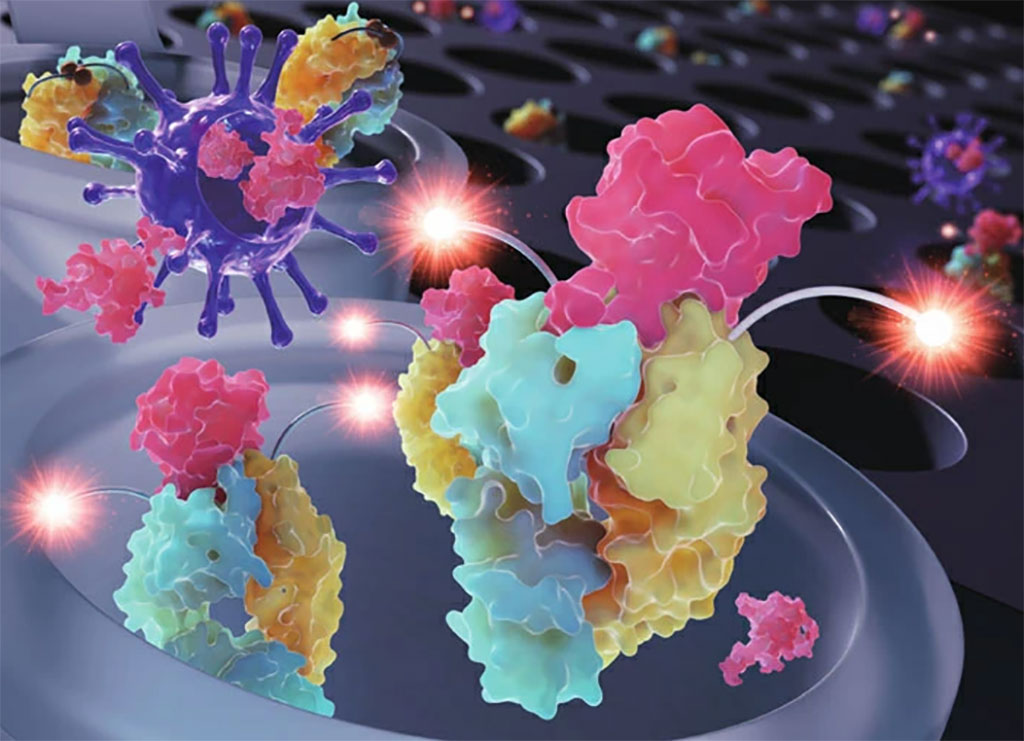
The incredibly fast spread of COVID-19 throughout the world brought to light a very important fact: we need better methods to diagnose infectious diseases quickly and efficiently. During the early months of the pandemic, polymerase chain reaction (PCR) tests were one of the most widely used techniques to detect COVID-19. However, these viral RNA-based techniques require expensive equipment and reaction times longer than an hour, which renders them less than ideal for point-of-care testing. The limitations of PCR fueled the development of various immunoassay methods, which use specially engineered antibodies to detect SARS-CoV-2 antigens with high sensitivity in little time. Today, scientists are still improving immunoassay technology to make available tools more convenient, sensitive, and cost-effective. Against this backdrop, a team of researchers has developed a new immunosensor based on Quenchbody technology that shows great potential as a fast, inexpensive, and convenient tool to detect SARS-CoV-2. This highly efficient diagnostic approach will be useful not only for point-of-care testing, but also for high-throughput epidemiological studies of COVID-19 and other emerging infectious diseases.
The team of researchers at Tokyo Institute of Technology (Tokyo Tech, Tokyo, Japan) has not only developed a new Quenchbody fluorescent immunosensor that can detect SARS-CoV-2 with exceptional speed and sensitivity, but also created a simple way to greatly enhance the immunosensor's performance using a crowding agent. A Quenchbody is a molecular sensor originally developed by Professor Ueda and colleagues using antibody fragments and fluorescent tags. The antibody fragment, which can be an antigen-binding region (or 'Fab'), targets a specific viral molecule (antigen). Meanwhile, the fluorescent tags are small fluorescent dye molecules attached by a peptide linker to the Quenchbody, near the antigen-binding region. When the antigen is absent, the fluorescent tags are attracted to the Fab and intrinsic amino acids (mainly tryptophan) interact with the dyes and quench the fluorescence. However, when the antigen appears, it replaces the fluorescent tag at the Fab, causing it to move away and recover its fluorescence. Thus, in a Quenchbody test, an increase in fluorescence indicates the detection of the target antigen.
In this study, the research team developed a double-tagged Quenchbody targeting the nucleocapsid protein (N protein) of SARS-CoV-2. To take things one step further, they also tested whether various commercially available compounds could improve the immunosensor's sensitivity and detection time. In particular, adding polyethylene glycol 6000 (PEG6000) at the right concentration as a crowding agent increased performance quite significantly. To further validate their approach, the team tested their immunosensor on leftover clinical samples from COVID-19 positive patients. After careful analysis of the results, they concluded that their newly developed Quenchbody could measure N protein more easily and quantitatively than a commercial lateral flow antigen test.
"Our work shows the feasibility of using Quenchbody immunosensors as rapid and cost-efficient tools for the diagnosis and high-throughput analysis of swab samples in large-scale monitoring and epidemiological studies of COVID-19, as well as other emerging infectious diseases," said Professor Hiroshi Ueda at Tokyo Tech who led the research.
Related Links:
Tokyo Tech
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel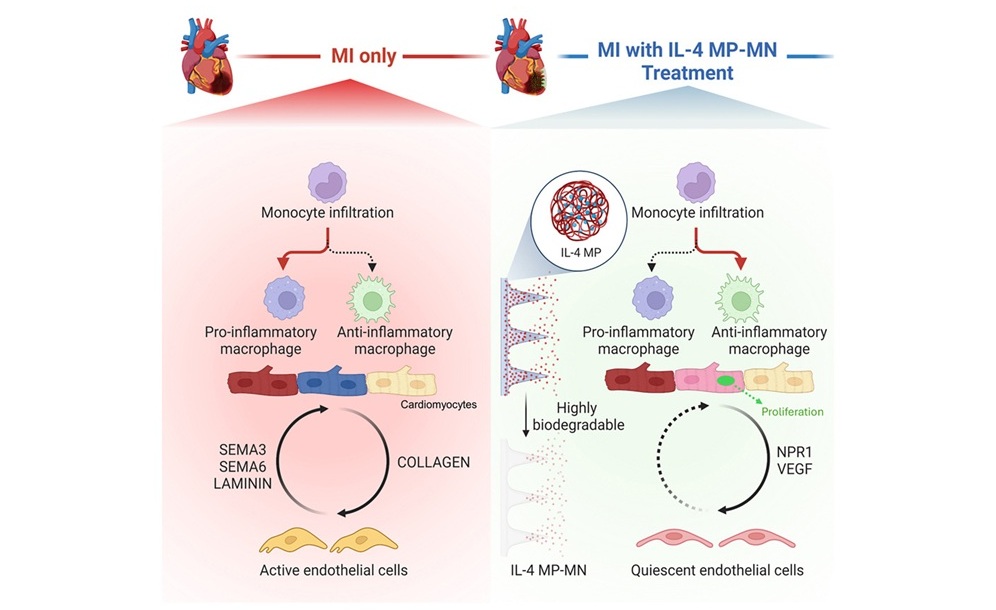
Biodegradable Patch Repairs Damaged Tissue After Heart Attack
A heart attack causes sudden loss of oxygen to the heart muscle, triggering cell death and a strong inflammatory response that often leads to scar formation. While scarring helps stabilize the heart, it... Read more
Magnetically Guided Microrobots to Enable Targeted Drug Delivery
Stroke affects 12 million people globally each year, often causing death or lasting disability. Current treatment relies on systemic administration of clot-dissolving drugs, which circulate throughout... Read more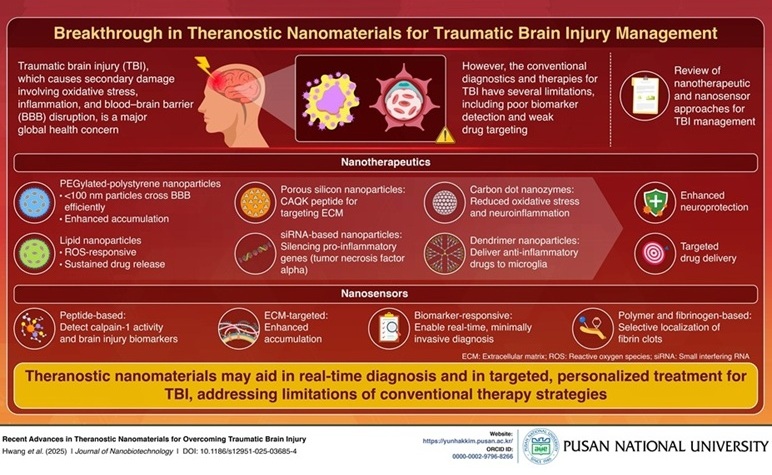
Smart Nanomaterials Detect and Treat Traumatic Brain Injuries Simultaneously
Traumatic brain injury (TBI) continues to leave millions with long-term disabilities every year. After a sudden impact from a fall, collision, or accident, the brain undergoes inflammation, oxidative stress,... Read more
Earlier Blood Transfusion Could Reduce Heart Failure and Arrhythmia in Heart Disease Patients
Blood loss during or after surgery can place significant stress on people with heart disease, increasing the risk of dangerous complications. Transfusions are often delayed until hemoglobin levels fall... Read moreSurgical Techniques
view channelNovel Endoscopy Technique Provides Access to Deep Lung Tumors
Detecting lung cancer early can save lives, but diagnosing small tumors deep in the outer regions of the lungs remains a major clinical challenge. Although CT scans frequently identify tiny suspicious... Read more
New Study Findings Could Halve Number of Stent Procedures
When a coronary artery becomes acutely blocked during a heart attack, opening it immediately is essential to prevent irreversible damage. However, many patients also have other narrowed vessels that appear... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more