Certain Blood Types Could Be Associated with Greater Risk of Contracting COVID-19, Confirms New Study
|
By HospiMedica International staff writers Posted on 04 Mar 2021 |
Illustration
As researchers around the world work to identify and address risk factors for severe COVID-19, there is additional evidence that certain blood types could be associated with greater risk of contracting the disease.
The findings of one of the first laboratory studies conducted by researchers at Brigham and Women’s Hospital (Boston, MA, USA) suggest that SARS-CoV-2, the virus that causes COVID-19, is particularly attracted to the blood group A antigen found on respiratory cells. In the study, researchers assessed a protein on the surface of the SARS-CoV-2 virus called the receptor binding domain, or RBD. The RBD is the part of the virus that attaches to the host cells, so it is an important research target for understanding how infection occurs. The team assessed synthetic blood group antigens on respiratory and red blood cells found in blood group A, B, and O individuals, and analyzed how the SARS-CoV-2 RBD interacted with each unique blood type. They discovered that the RBD had a strong preference for binding to blood group A found on respiratory cells. It did not display a preference for blood group A red blood cells, or other blood groups found on respiratory or red cells. The capacity of the RBD to preferentially recognize and attach to the blood type A antigen found in the lungs of blood type A individuals may provide insight into the potential link between blood group A and COVID-19 infection.
Based on their observations, the team sought to determine whether a similar binding preference existed for the RBD of SARS-CoV, the virus that causes severe acute respiratory syndrome (SARS). Although the makeup of the virus differs, the SARS-CoV RBD exhibited the same preference to bind to the group A antigens on respiratory cells. The team has emphasized that their findings alone could not fully describe or predict how coronaviruses like SARS-CoV-2 and SARS-CoV would affect patients of various blood types. While further research is needed to understand that influence, the research adds to findings from earlier studies suggesting a possible link between blood type and COVID-19 susceptibility and severity.
“It is interesting that the viral RBD only really prefers the type of blood group A antigens that are on respiratory cells, which are presumably how the virus is entering most patients and infecting them,” said study author Sean R. Stowell, MD, PhD, of Brigham and Women’s Hospital. “Blood type is a challenge because it is inherited and not something we can change. But if we can better understand how the virus interacts with blood groups in people, we may be able to find new medicines or methods of prevention.”
Related Links:
Brigham and Women’s Hospital
The findings of one of the first laboratory studies conducted by researchers at Brigham and Women’s Hospital (Boston, MA, USA) suggest that SARS-CoV-2, the virus that causes COVID-19, is particularly attracted to the blood group A antigen found on respiratory cells. In the study, researchers assessed a protein on the surface of the SARS-CoV-2 virus called the receptor binding domain, or RBD. The RBD is the part of the virus that attaches to the host cells, so it is an important research target for understanding how infection occurs. The team assessed synthetic blood group antigens on respiratory and red blood cells found in blood group A, B, and O individuals, and analyzed how the SARS-CoV-2 RBD interacted with each unique blood type. They discovered that the RBD had a strong preference for binding to blood group A found on respiratory cells. It did not display a preference for blood group A red blood cells, or other blood groups found on respiratory or red cells. The capacity of the RBD to preferentially recognize and attach to the blood type A antigen found in the lungs of blood type A individuals may provide insight into the potential link between blood group A and COVID-19 infection.
Based on their observations, the team sought to determine whether a similar binding preference existed for the RBD of SARS-CoV, the virus that causes severe acute respiratory syndrome (SARS). Although the makeup of the virus differs, the SARS-CoV RBD exhibited the same preference to bind to the group A antigens on respiratory cells. The team has emphasized that their findings alone could not fully describe or predict how coronaviruses like SARS-CoV-2 and SARS-CoV would affect patients of various blood types. While further research is needed to understand that influence, the research adds to findings from earlier studies suggesting a possible link between blood type and COVID-19 susceptibility and severity.
“It is interesting that the viral RBD only really prefers the type of blood group A antigens that are on respiratory cells, which are presumably how the virus is entering most patients and infecting them,” said study author Sean R. Stowell, MD, PhD, of Brigham and Women’s Hospital. “Blood type is a challenge because it is inherited and not something we can change. But if we can better understand how the virus interacts with blood groups in people, we may be able to find new medicines or methods of prevention.”
Related Links:
Brigham and Women’s Hospital
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
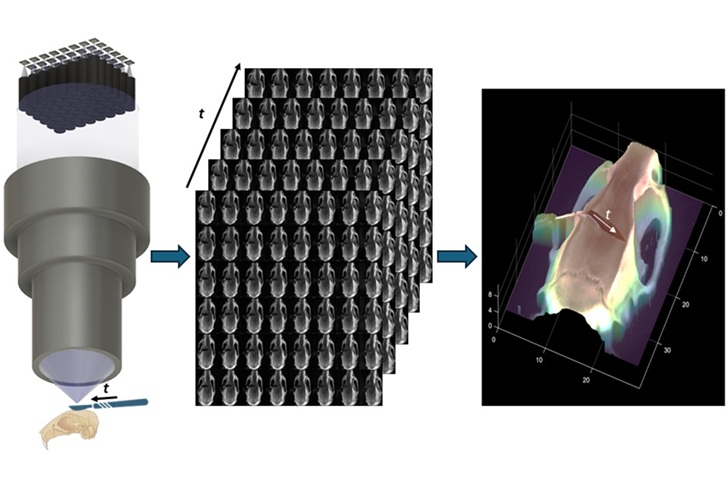
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel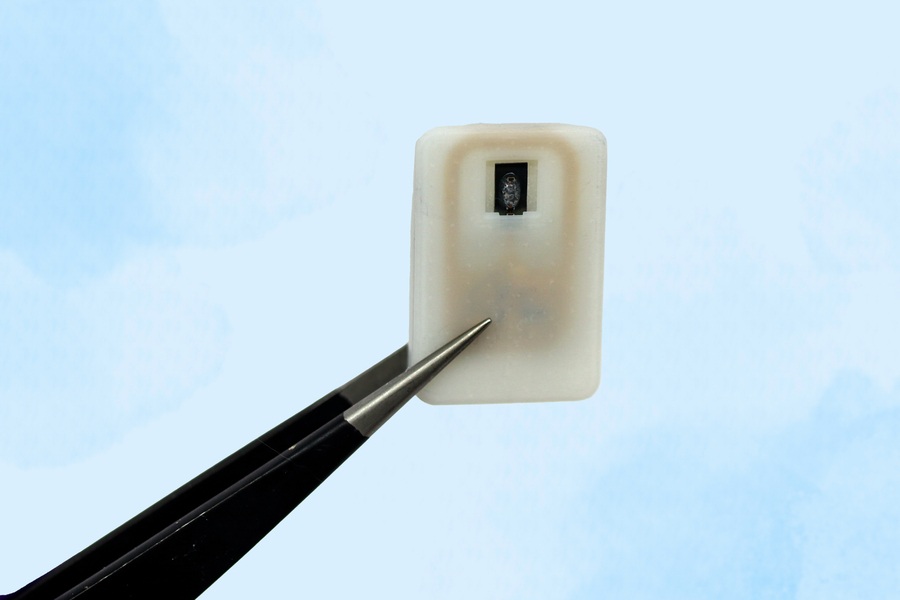
Implantable Device Could Save Diabetes Patients from Dangerously Low Blood Sugar
For individuals with Type 1 diabetes, hypoglycemia (low blood sugar) presents a life-threatening threat, particularly when glucose levels drop too low, which can result in seizures, coma, or even death.... Read more
New Prostate Screening Device Could Replace Traditional Examination Method
Prostate cancer is a leading health concern, with one in seven men being diagnosed with the disease. Early detection is critical for improving patient outcomes, but traditional diagnostic methods, such... Read moreSurgical Techniques
view channel
Fluorescent Imaging Agent ‘Lights Up’ Nerves for Better Visualization During Surgery
Surgical nerve injury is a significant concern in head and neck surgeries, where nerves are at risk of being inadvertently damaged during procedures. Such injuries can lead to complications that may impact... Read more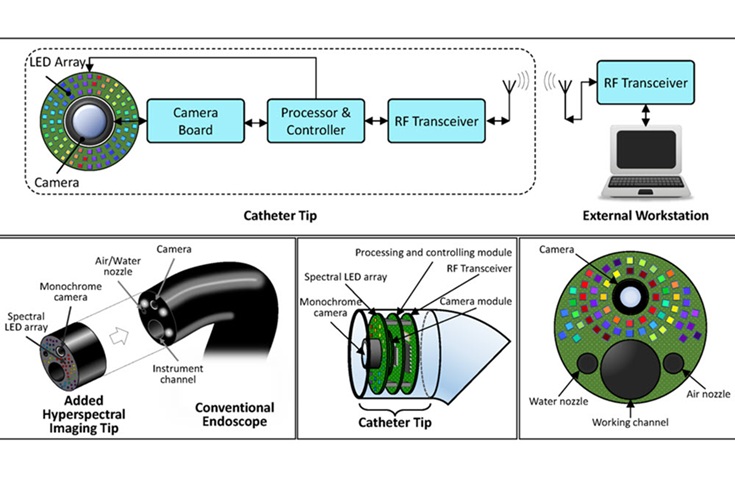
LED-Based Imaging System Could Transform Cancer Detection in Endoscopy
Gastrointestinal cancers remain one of the most common and challenging forms of cancer to diagnose accurately. Despite the widespread use of endoscopy for screening and diagnosis, the procedure still misses... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Bayer and Broad Institute Extend Research Collaboration to Develop New Cardiovascular Therapies
A research collaboration will focus on the joint discovery of novel therapeutic approaches based on findings in human genomics research related to cardiovascular diseases. Bayer (Berlin, Germany) and... Read more