New Treatment Based on Natural Molecules That Improves Lung Function Could Keep COVID-19 Patients Off Ventilator
|
By HospiMedica International staff writers Posted on 28 Apr 2021 |

Illustration
A new treatment is among the first known to reduce the severity of acute respiratory distress syndrome (ARDS) caused by the flu in animals and could also keep COVID-19 patients off the ventilator.
Tests done by researchers at The Ohio State University (Columbus, OH, USA) in mice infected with high doses of influenza showed that the treatment could improve lung function in very sick mice and prevent progression of disease in mice that were pre-emptively treated after being exposed to the flu. The hope is that it may also help humans infected with the flu, and potentially other causes of ARDS) such as SARS-CoV-2 infection.
Specific cells in mice are less able to make key molecules after influenza invades the lungs, reducing their ability to produce a substance called surfactant that enables lungs to expand and contract. The shortage of surfactant is linked to ARDS, an illness so serious that it typically requires mechanical ventilation in an ICU. Researchers bypassed the blocked process in mice by re-introducing the missing molecules alone or in combination as an injected or oral treatment. The results: normalized blood oxygen levels and reduced inflammation in mouse lungs - effects that could make a person well enough for hospital discharge.
ARDS can also result from infections, cancer, trauma and many other ailments. Though this therapy has been tested in the context of the flu, its reliance on fixing a broken cell function in the host rather than killing the virus suggests it has potential to treat virtually any lung injury. The experimental treatment consists of molecules known as liponucleotides, which are essential for making surfactant in the lungs. The researchers analyzed lung cells from flu-infected mice and determined that the pathway to surfactant production was disrupted, with one of the two necessary liponucleotides completely undetectable.
The team fixed this in mice by developing therapies containing the missing liponucleotide molecule alone or combined with one or two others. The researchers inoculated mice with high doses of H1N1 influenza and then treated some mice with liponucleotides once daily for five days and others just a single time five days after exposure. The mice receiving daily treatment were protected from getting seriously ill, and the very sick mice treated on the fifth day, whose severe blood-oxygen loss and lung inflammation had cause ARDS, showed significant improvement.
There’s still a lot to learn. The agents have a strong anti-inflammatory effect, but don’t fully restore the surfactant-production process and the researchers are still not sure why that is. Studies so far have been based on findings in a single type of lung cell, but the researchers haven’t confirmed that those cells are the ones responding to the therapy - any number of other cells in the immune system, blood vessels or heart could also play a role. Despite the unknowns, the researchers believe that the missing liponucleotides naturally exist in mammals, including humans, they are considered safe and unlikely to cause side effects, even if they go unused in the body.
“The most important and impressive thing in this study is the fact that we have benefits even when we treat late in the disease process. If we could develop a drug based on these findings, you could take somebody who’s going to have to go on a ventilator and stop that completely,” said Ian Davis, professor of veterinary biosciences at The Ohio State University and senior author of the study. “There’s nothing out there now that can do this for ARDS that will bring them back to that degree, and certainly not for flu.”
Related Links:
The Ohio State University
Tests done by researchers at The Ohio State University (Columbus, OH, USA) in mice infected with high doses of influenza showed that the treatment could improve lung function in very sick mice and prevent progression of disease in mice that were pre-emptively treated after being exposed to the flu. The hope is that it may also help humans infected with the flu, and potentially other causes of ARDS) such as SARS-CoV-2 infection.
Specific cells in mice are less able to make key molecules after influenza invades the lungs, reducing their ability to produce a substance called surfactant that enables lungs to expand and contract. The shortage of surfactant is linked to ARDS, an illness so serious that it typically requires mechanical ventilation in an ICU. Researchers bypassed the blocked process in mice by re-introducing the missing molecules alone or in combination as an injected or oral treatment. The results: normalized blood oxygen levels and reduced inflammation in mouse lungs - effects that could make a person well enough for hospital discharge.
ARDS can also result from infections, cancer, trauma and many other ailments. Though this therapy has been tested in the context of the flu, its reliance on fixing a broken cell function in the host rather than killing the virus suggests it has potential to treat virtually any lung injury. The experimental treatment consists of molecules known as liponucleotides, which are essential for making surfactant in the lungs. The researchers analyzed lung cells from flu-infected mice and determined that the pathway to surfactant production was disrupted, with one of the two necessary liponucleotides completely undetectable.
The team fixed this in mice by developing therapies containing the missing liponucleotide molecule alone or combined with one or two others. The researchers inoculated mice with high doses of H1N1 influenza and then treated some mice with liponucleotides once daily for five days and others just a single time five days after exposure. The mice receiving daily treatment were protected from getting seriously ill, and the very sick mice treated on the fifth day, whose severe blood-oxygen loss and lung inflammation had cause ARDS, showed significant improvement.
There’s still a lot to learn. The agents have a strong anti-inflammatory effect, but don’t fully restore the surfactant-production process and the researchers are still not sure why that is. Studies so far have been based on findings in a single type of lung cell, but the researchers haven’t confirmed that those cells are the ones responding to the therapy - any number of other cells in the immune system, blood vessels or heart could also play a role. Despite the unknowns, the researchers believe that the missing liponucleotides naturally exist in mammals, including humans, they are considered safe and unlikely to cause side effects, even if they go unused in the body.
“The most important and impressive thing in this study is the fact that we have benefits even when we treat late in the disease process. If we could develop a drug based on these findings, you could take somebody who’s going to have to go on a ventilator and stop that completely,” said Ian Davis, professor of veterinary biosciences at The Ohio State University and senior author of the study. “There’s nothing out there now that can do this for ARDS that will bring them back to that degree, and certainly not for flu.”
Related Links:
The Ohio State University
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
Implantable Device Could Save Diabetes Patients from Dangerously Low Blood Sugar
For individuals with Type 1 diabetes, hypoglycemia (low blood sugar) presents a life-threatening threat, particularly when glucose levels drop too low, which can result in seizures, coma, or even death.... Read more
New Prostate Screening Device Could Replace Traditional Examination Method
Prostate cancer is a leading health concern, with one in seven men being diagnosed with the disease. Early detection is critical for improving patient outcomes, but traditional diagnostic methods, such... Read moreSurgical Techniques
view channel
Fluorescent Imaging Agent ‘Lights Up’ Nerves for Better Visualization During Surgery
Surgical nerve injury is a significant concern in head and neck surgeries, where nerves are at risk of being inadvertently damaged during procedures. Such injuries can lead to complications that may impact... Read more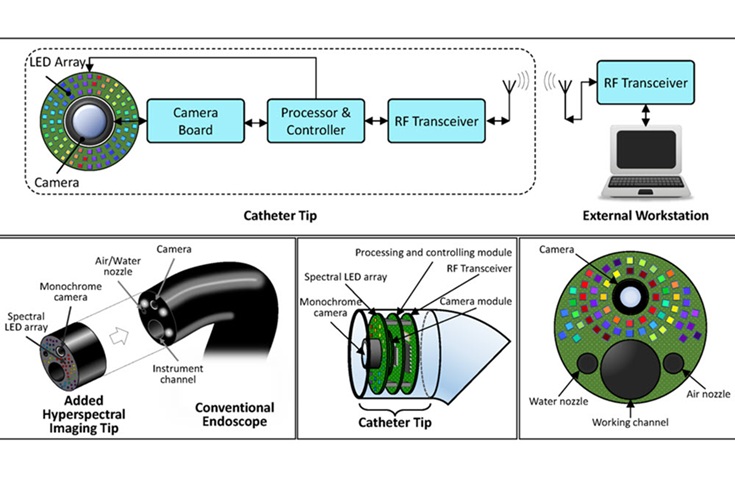
LED-Based Imaging System Could Transform Cancer Detection in Endoscopy
Gastrointestinal cancers remain one of the most common and challenging forms of cancer to diagnose accurately. Despite the widespread use of endoscopy for screening and diagnosis, the procedure still misses... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Bayer and Broad Institute Extend Research Collaboration to Develop New Cardiovascular Therapies
A research collaboration will focus on the joint discovery of novel therapeutic approaches based on findings in human genomics research related to cardiovascular diseases. Bayer (Berlin, Germany) and... Read more