Trauma Center Closure Increases Mortality Risk
|
By HospiMedica International staff writers Posted on 09 Apr 2014 |
A new study reveals a strong association between closure of trauma centers and increased mortality for patients with injuries.
Researchers at the University of California, San Francisco (UCSF; USA) performed a retrospective study of all adult patient visits for injuries at Level I and II to nonfederal trauma centers in California (USA) between 1999 and 2009, to examine the impact of three trauma center closures. The researchers compared the in-hospital mortality of 5,122 patients who lived in ZIP [US postal] codes where their drive time to that nearest trauma center increased as the result of a nearby closure to 228,236 patients whose drive time did not change, and 37,787 patients whose travel time decreased as the result of a trauma center opening. They also tested whether this effect was limited to a two-year period following a closure.
The results showed that decreased travel time to the closest trauma center was associated with 17% lower odds of in-hospital mortality compared to the group experiencing no change, while increased travel time was associated with 14% higher odds of in-hospital mortality. These effects were intensified in the first two years following a closure. Injured patients with decreased travel times to the nearest trauma center had 16% lower odds of death, while injured patients affected by a closure had 26% higher odds of death. The article was published in the March 2014 issue of the Journal of Trauma and Acute Care Surgery.
“This study confirms that when trauma centers close, people who live in the surrounding areas are more likely to die following an injury,” said lead author Renee Hsia, MD, an associate professor of emergency medicine at UCSF. “Affected patients were more likely to be young and low income, to identify as part of a racial or ethnic minority group, and have medical insurance.”
Trauma centers are an effective but costly element of the US health care infrastructure. Some Level I and II trauma centers regularly incur financial losses when these high fixed costs are coupled with high burdens of uncompensated care for disproportionately young and uninsured trauma patients. As a result, they are at risk of reducing their services or closing.
Related Links:
University of California, San Francisco
Researchers at the University of California, San Francisco (UCSF; USA) performed a retrospective study of all adult patient visits for injuries at Level I and II to nonfederal trauma centers in California (USA) between 1999 and 2009, to examine the impact of three trauma center closures. The researchers compared the in-hospital mortality of 5,122 patients who lived in ZIP [US postal] codes where their drive time to that nearest trauma center increased as the result of a nearby closure to 228,236 patients whose drive time did not change, and 37,787 patients whose travel time decreased as the result of a trauma center opening. They also tested whether this effect was limited to a two-year period following a closure.
The results showed that decreased travel time to the closest trauma center was associated with 17% lower odds of in-hospital mortality compared to the group experiencing no change, while increased travel time was associated with 14% higher odds of in-hospital mortality. These effects were intensified in the first two years following a closure. Injured patients with decreased travel times to the nearest trauma center had 16% lower odds of death, while injured patients affected by a closure had 26% higher odds of death. The article was published in the March 2014 issue of the Journal of Trauma and Acute Care Surgery.
“This study confirms that when trauma centers close, people who live in the surrounding areas are more likely to die following an injury,” said lead author Renee Hsia, MD, an associate professor of emergency medicine at UCSF. “Affected patients were more likely to be young and low income, to identify as part of a racial or ethnic minority group, and have medical insurance.”
Trauma centers are an effective but costly element of the US health care infrastructure. Some Level I and II trauma centers regularly incur financial losses when these high fixed costs are coupled with high burdens of uncompensated care for disproportionately young and uninsured trauma patients. As a result, they are at risk of reducing their services or closing.
Related Links:
University of California, San Francisco
Latest Hospital News News
- Nurse Tracking System Improves Hospital Workflow
- New Children’s Hospital Transforms California Healthcare
- Noisy Hospitals Face Threat of Decreased Federal Compensation
- Orthopedics Centre of Excellence Planned for Guy’s Hospital
- Research Suggests Avoidance of Low-Value Surgical Procedures
- U.S. Federal Readmission Fines Linked to Higher Mortality
- Columbia China to Build New Hospital in Jiaxing
- Dubai Debuts Second Robotic Pharmacy Service
- Seattle Hospital Network Shifts Away from Overlapping Surgeries
- ACC to Launch Valvular Heart Disease Program in China
- Mortality Rates Lower at Major Teaching Hospitals
- South Australia to Inaugurate Upscale Hospital
- Raffles to Launch Second Hospital Project in China
- Research Center Tackles Antimicrobial Drugs Challenge
- Miami Cardiac & Vascular Institute Completes Expansion Project
- Hospital Antibiotic Policies Improve Prescription Practices
Channels
Artificial Intelligence
view channelCritical Care
view channel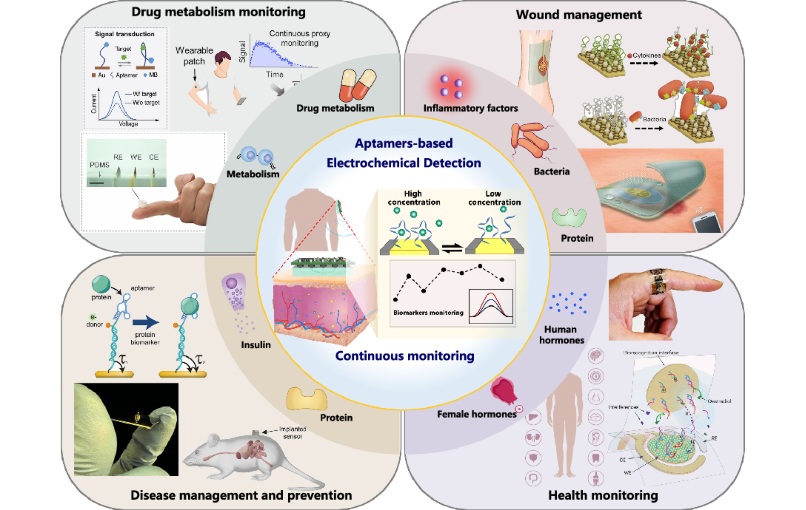
Aptamers Enable Real-Time Biomarker Tracking Without Blood Draws
Continuous monitoring of biomarkers is critical for early disease detection, treatment evaluation, and personalized health management. Yet most clinical tests still rely on invasive, single-point blood... Read more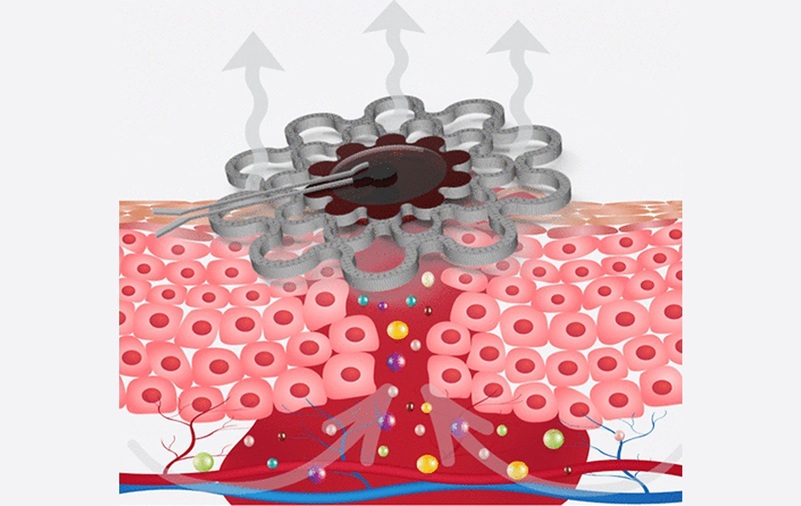
Specialized Dressing with Sensor Monitors pH Levels in Chronic Wounds
Any wound has the potential to become chronic, but the risk is significantly higher in individuals with certain medical conditions. Once a wound becomes chronic, healing slows, complications increase,... Read moreSurgical Techniques
view channel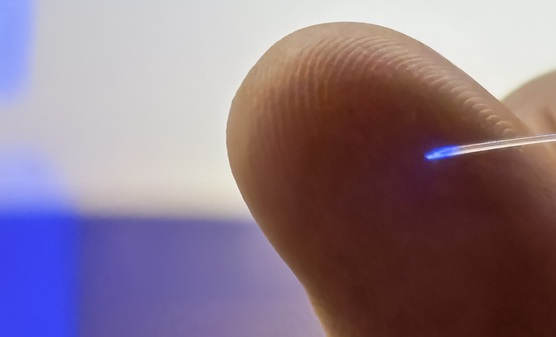
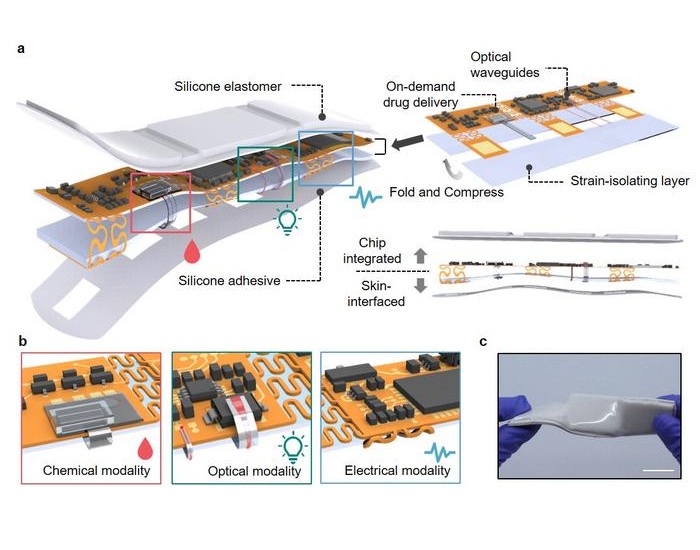
Brain Implant Records Neural Signals and Delivers Precise Medication
Neurological diseases such as epilepsy involve complex interactions across multiple layers of the brain, yet current implants can typically stimulate or record activity from only a single point.... Read moreAI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
Lipid-rich plaques inside coronary arteries are strongly associated with heart attacks and other major cardiac events. While optical coherence tomography (OCT) provides detailed images of vessel structure... Read moreNeural Device Regrows Surrounding Skull After Brain Implantation
Placing electronic implants on the brain typically requires removing a portion of the skull, creating challenges for long-term access and safe closure. Current methods often involve temporarily replacing the skull or securing metal plates, which can lead to complications such as skin erosion and additional surgeries.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more