Children's Hospitals Are Being Fined Unequally for Readmissions
|
By HospiMedica International staff writers Posted on 01 Mar 2016 |
A new study finds that pay-for-performance (P4P) measures might penalize hospitals treating children from deprived or ethnically backward minorities in an unequal way, due to factors beyond their control.
Researchers at the University of Colorado (Aurora, USA), the Children’s Hospital Association (Overland Park, KS, USA), and other institutions conducted a retrospective cohort study of 43 free-standing children’s hospitals within the Pediatric Health Information System database to determine whether risk adjustment for commonly available social determinants of health (SDH) affects the readmissions-based P4P penalty status of children’s hospitals in the United States.
The researchers examined hospital discharges from 2013 that met criteria for potentially preventable readmissions, and evaluated two risk-adjustment models. The first was a baseline model adjusted for severity of illness. The second was an SDH-enhanced model that adjusted for severity of illness and a set of four variables that included race, ethnicity, payer, and the median household income for the patient’s home zip code. The main outcome was the change in a hospital’s potentially preventable readmissions penalty status.
Data from 179,400 hospital discharges at the 43 hospitals showed that SDH variables were distributed per 39.2% nonwhite, 17.9% Hispanic, and 58.7% publicly insured; median household income for the patient’s home zip code was USD 40,674. When compared with the baseline model, adjustment for SDH resulted in a change in penalty status for three hospitals within the 15-day readmission window, and five hospitals within the 30-day window. The study was published on February 15, 2016, in JAMA Pediatrics.
“Studies like ours show that patients who are poorer or are minorities are readmitted at higher rates than other patients,” said lead author Marion Sills, MD, of the University of Colorado, “which raises concern that the readmissions penalties punish hospitals for the type of patients that they serve, rather than purely for the quality of care they provide.”
Medicare (Baltimore, MD, USA) launched the penalty program in 2012 in an attempt to combat a perverse financial incentive, wherein hospitals earned more money if patients were readmitted to health deterioration after they are discharged, because they can be paid for two stays instead of one. In 2013 Medicare levied fines of USD 227 million against 2,225 hospitals that had their payments reduced by up to 2% the following year.
Related Links:
University of Colorado
Children’s Hospital Association
Medicare
Researchers at the University of Colorado (Aurora, USA), the Children’s Hospital Association (Overland Park, KS, USA), and other institutions conducted a retrospective cohort study of 43 free-standing children’s hospitals within the Pediatric Health Information System database to determine whether risk adjustment for commonly available social determinants of health (SDH) affects the readmissions-based P4P penalty status of children’s hospitals in the United States.
The researchers examined hospital discharges from 2013 that met criteria for potentially preventable readmissions, and evaluated two risk-adjustment models. The first was a baseline model adjusted for severity of illness. The second was an SDH-enhanced model that adjusted for severity of illness and a set of four variables that included race, ethnicity, payer, and the median household income for the patient’s home zip code. The main outcome was the change in a hospital’s potentially preventable readmissions penalty status.
Data from 179,400 hospital discharges at the 43 hospitals showed that SDH variables were distributed per 39.2% nonwhite, 17.9% Hispanic, and 58.7% publicly insured; median household income for the patient’s home zip code was USD 40,674. When compared with the baseline model, adjustment for SDH resulted in a change in penalty status for three hospitals within the 15-day readmission window, and five hospitals within the 30-day window. The study was published on February 15, 2016, in JAMA Pediatrics.
“Studies like ours show that patients who are poorer or are minorities are readmitted at higher rates than other patients,” said lead author Marion Sills, MD, of the University of Colorado, “which raises concern that the readmissions penalties punish hospitals for the type of patients that they serve, rather than purely for the quality of care they provide.”
Medicare (Baltimore, MD, USA) launched the penalty program in 2012 in an attempt to combat a perverse financial incentive, wherein hospitals earned more money if patients were readmitted to health deterioration after they are discharged, because they can be paid for two stays instead of one. In 2013 Medicare levied fines of USD 227 million against 2,225 hospitals that had their payments reduced by up to 2% the following year.
Related Links:
University of Colorado
Children’s Hospital Association
Medicare
Latest Hospital News News
- Nurse Tracking System Improves Hospital Workflow
- New Children’s Hospital Transforms California Healthcare
- Noisy Hospitals Face Threat of Decreased Federal Compensation
- Orthopedics Centre of Excellence Planned for Guy’s Hospital
- Research Suggests Avoidance of Low-Value Surgical Procedures
- U.S. Federal Readmission Fines Linked to Higher Mortality
- Columbia China to Build New Hospital in Jiaxing
- Dubai Debuts Second Robotic Pharmacy Service
- Seattle Hospital Network Shifts Away from Overlapping Surgeries
- ACC to Launch Valvular Heart Disease Program in China
- Mortality Rates Lower at Major Teaching Hospitals
- South Australia to Inaugurate Upscale Hospital
- Raffles to Launch Second Hospital Project in China
- Research Center Tackles Antimicrobial Drugs Challenge
- Miami Cardiac & Vascular Institute Completes Expansion Project
- Hospital Antibiotic Policies Improve Prescription Practices
Channels
Artificial Intelligence
view channelCritical Care
view channel
3D-Printed Bandage to Help Heal Chronic Wounds
Chronic wounds such as diabetic ulcers and pressure sores can persist for months or even years, especially in people with diabetes or limited mobility. These wounds often receive poor oxygen supply, slowing... Read more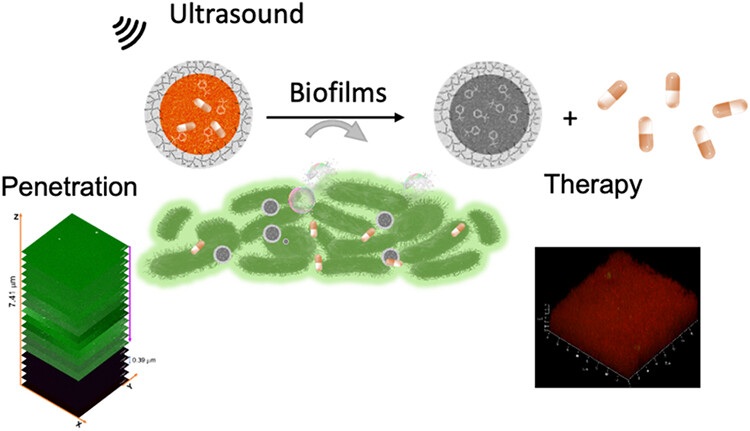
Ultrasound-Activated Nanoagents Kill Superbugs Hiding in Biofilms
Bacterial infections that form biofilms are notoriously difficult to treat. These dense, protective microbial layers shield bacteria from antibiotics and the immune system, often leading to persistent... Read moreSurgical Techniques
view channel
Minimally Invasive Procedure Effectively Treats Small Kidney Cancers
Small kidney cancers are increasingly detected during routine CT scans performed for other medical evaluations. These early-stage tumors, classified as T1a renal cell carcinoma, are typically treated with... Read more
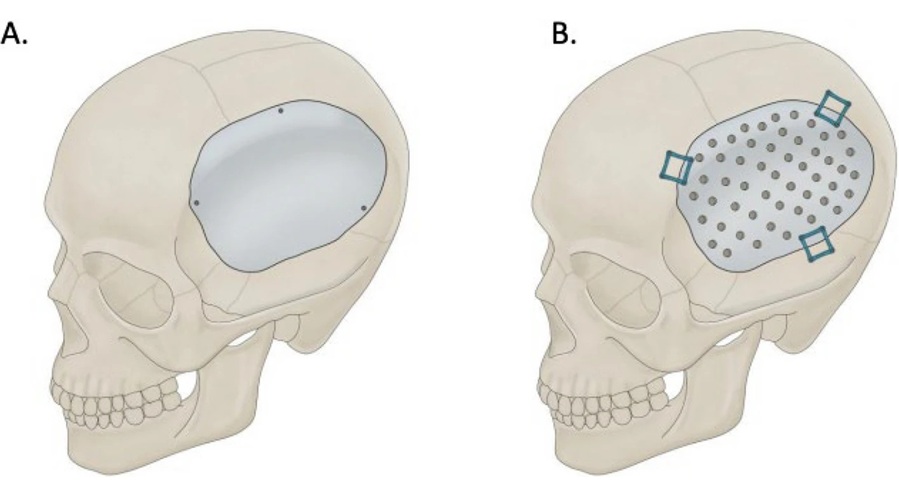
Neurostimulation Implant Reduces Seizure Burden in Drug-Resistant Epilepsy
Drug-resistant focal epilepsy leaves many patients with persistent seizures despite medication, exposing them to injury risk and reduced quality of life. Traditional surgical options are invasive and can... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more