Polymer Implant Delivers Drugs to Pancreatic Tumors
|
By HospiMedica International staff writers Posted on 28 Apr 2016 |

Image: The paclitaxel-delivering PLGA polymer film (Photo courtesy of Bryce Vickmark, MIT).
A novel implantable delivery platform can provide local chemotherapy for treating pancreatic ductal adenocarcinoma (PDAC), according to a new study.
Developed by researchers at the Massachusetts Institute of Technology (MIT, Cambridge, MA, USA) and Massachusetts General Hospital (MGH; Boston, MA, USA), the implant is a biodegradable polymer flexible film made of poly lactic-co-glycolic acid (PLGA), and is designed to release high doses of chemotherapeutic drugs for up to 60 days. For delivery, the film is rolled into a tube and inserted through a catheter; once it reaches the pancreas, it unfolds and conforms to the shape of the tumor, releasing the embedded drugs only from the tumor-facing side to reduce side effects.
To compare the device's efficacy to that of traditional chemotherapy, a study was conducted in mice carrying human pancreatic tumors. One group of mice was treated with the implant carrying the chemo drug paclitaxel, while the other group received injections of the same drug for four weeks, simulating current treatment for human patients. The results showed that tumor growth slowed in mice with the implant; in some cases, the tumors even shrank. After four weeks, the implant group showed five times the paclitaxel concentration in their tumors that the intravenous group did.
In addition to successfully delivering the drug to the pancreas, the researchers also observed other positive effects. The localized treatment increased the amount of necrotic tissue, and since there are few blood vessels in pancreatic tumors, the paclitaxel tended to remain in-situ, preventing toxic effects in healthy tissues. Additionally, by acting as a physical barrier, the film was able to reduce metastasis to nearby organs. The study describing the implant and the murine study was published early online on March 31, 2016, in Biomaterials.
“The greatest benefit of this device is the ability to implant it with minimally invasive procedures, so we can give a tool to oncologists and surgeons to reach tumors that otherwise would be difficult to reach,” said lead author Laura Indolfi, PhD, of the MIT Institute for Medical Engineering and Science (IMES) and the MGH Cancer Center. “You can implant our device to achieve a localized drug release to control tumor progression and potentially shrink the tumor to a size where a surgeon can remove it.”
Pancreatic cancer patients often suffer from blockage of the bile duct, which interferes with digestion and is very painful. The duct can be reopened with a stent, but usually gets blocked again, requiring the patient to have the old stent removed and a new one inserted. According to the researchers, the film could also be used as a coating for such a stent, helping to prevent the cancer cells from spreading into the bile duct and blocking it again.
Related Links:
Massachusetts Institute of Technology
Massachusetts General Hospital
Developed by researchers at the Massachusetts Institute of Technology (MIT, Cambridge, MA, USA) and Massachusetts General Hospital (MGH; Boston, MA, USA), the implant is a biodegradable polymer flexible film made of poly lactic-co-glycolic acid (PLGA), and is designed to release high doses of chemotherapeutic drugs for up to 60 days. For delivery, the film is rolled into a tube and inserted through a catheter; once it reaches the pancreas, it unfolds and conforms to the shape of the tumor, releasing the embedded drugs only from the tumor-facing side to reduce side effects.
To compare the device's efficacy to that of traditional chemotherapy, a study was conducted in mice carrying human pancreatic tumors. One group of mice was treated with the implant carrying the chemo drug paclitaxel, while the other group received injections of the same drug for four weeks, simulating current treatment for human patients. The results showed that tumor growth slowed in mice with the implant; in some cases, the tumors even shrank. After four weeks, the implant group showed five times the paclitaxel concentration in their tumors that the intravenous group did.
In addition to successfully delivering the drug to the pancreas, the researchers also observed other positive effects. The localized treatment increased the amount of necrotic tissue, and since there are few blood vessels in pancreatic tumors, the paclitaxel tended to remain in-situ, preventing toxic effects in healthy tissues. Additionally, by acting as a physical barrier, the film was able to reduce metastasis to nearby organs. The study describing the implant and the murine study was published early online on March 31, 2016, in Biomaterials.
“The greatest benefit of this device is the ability to implant it with minimally invasive procedures, so we can give a tool to oncologists and surgeons to reach tumors that otherwise would be difficult to reach,” said lead author Laura Indolfi, PhD, of the MIT Institute for Medical Engineering and Science (IMES) and the MGH Cancer Center. “You can implant our device to achieve a localized drug release to control tumor progression and potentially shrink the tumor to a size where a surgeon can remove it.”
Pancreatic cancer patients often suffer from blockage of the bile duct, which interferes with digestion and is very painful. The duct can be reopened with a stent, but usually gets blocked again, requiring the patient to have the old stent removed and a new one inserted. According to the researchers, the film could also be used as a coating for such a stent, helping to prevent the cancer cells from spreading into the bile duct and blocking it again.
Related Links:
Massachusetts Institute of Technology
Massachusetts General Hospital
Latest Surgical Techniques News
- Microgrippers For Miniature Biopsies to Create New Cancer Diagnostic Screening Paradigm
- Miniature Soft Lithium-Ion Battery Could Be Used as Defibrillator During Surgery
- TAVI Procedure Supported by Radial Artery Access Reduces Bleeding Complications
- Portable Surgical Robot Seamlessly Integrates into Any OR for Performing Cholecystectomy Procedures
- New Thoracic Surgery Risk Calculators Support Preoperative Decision-Making
- Surgical Platform with Miniature Humanoid-Shaped Robotic Arms Provides Human Level Dexterity
- Precision Surgical Technique Enables Lymph Node Detection and Removal in Endometrial Cancer
- Glowing Approach Helps Surgeons Assess Neural Blood Flow in Chronic Nerve Compression Neuropathy
- Predictive Model Identifies Best Patients for Minimally Invasive Epilepsy Surgery
- Light-Driven Micro-Robot Designed to Swim Autonomously in Viscous Liquids Could Be Used for Unblocking Blood Vessels
- Novel Approach Combines Advanced Robotics and Low-Field MRI Technology for Incisionless Prostate Surgery
- Fast OCT System Integrated into Neurosurgical Microscope Identifies Tumor Margins During Brain Surgery
- Miniature Robots Transport Instruments for Endoscopic Microsurgery Through Body
- Robotic Visualization System for Neurosurgery Offers Greater Clarity for Complex Procedures
- Endometrial Ablation for Abnormal Uterine Bleeding Associated with High Risk of Hysterectomy
- Breakthrough Robot Technology Could Allow Entire Surgery to Be Performed Without Human Intervention
Channels
Critical Care
view channel_1.jpg)
Cutting-Edge Bioelectronic Device Offers Drug-Free Approach to Managing Bacterial Infections
Antibiotic-resistant infections pose an increasing threat to patient safety and healthcare systems worldwide. Recent estimates indicate that drug-resistant infections may rise by 70% by 2050, highlighting... Read more
Sophisticated Machine-Learning Approach Uses Patient EHRs to Predict Pneumonia Outcomes
Pneumonia, an infection that results in difficulty breathing due to fluid accumulation in the lungs, is one of the leading causes of death worldwide. This condition is particularly challenging to treat... Read more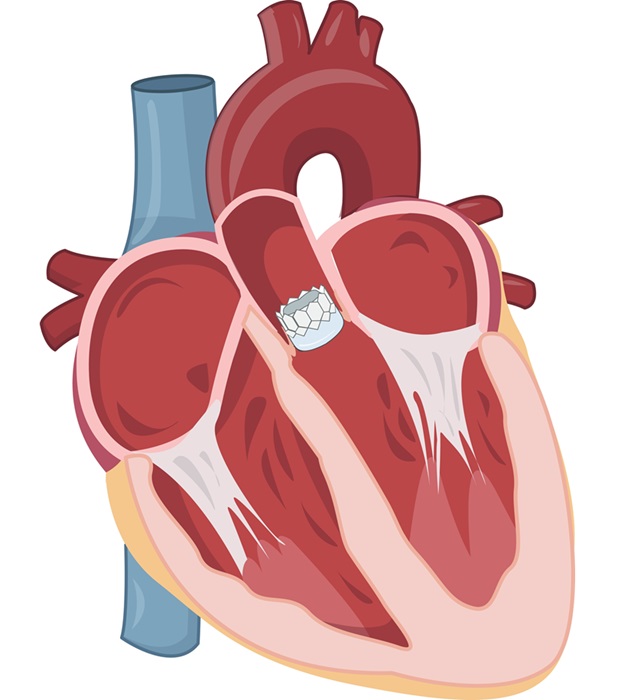
Early TAVR Benefits Patients with Asymptomatic Severe Aortic Stenosis
For patients with asymptomatic severe aortic stenosis (AS) and preserved left-ventricular ejection fraction, current guidelines recommend clinical surveillance every six to twelve months.... Read more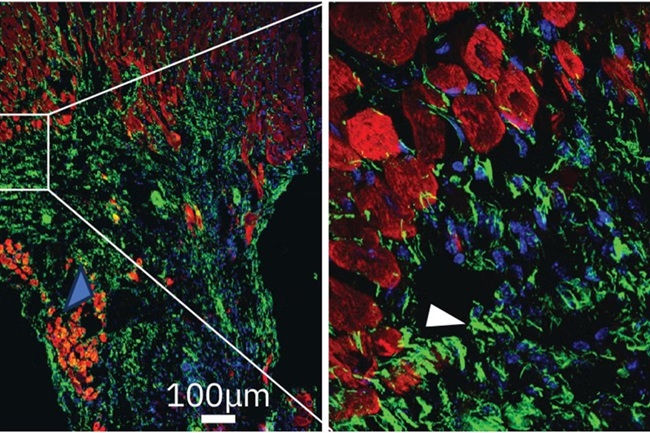
First-Of-Its-Kind Experimental Therapy Enhances Tissue Repair After Heart Attack
Cardiovascular disease remains the leading cause of death worldwide, accounting for one-third of all annual fatalities. Following a heart attack, the heart's natural regenerative ability is limited, resulting... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel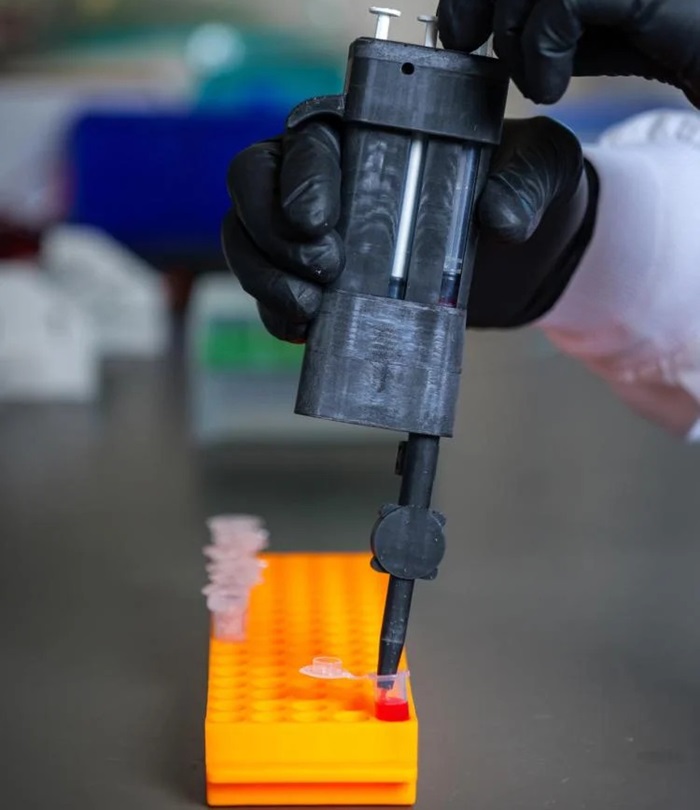
Handheld, Sound-Based Diagnostic System Delivers Bedside Blood Test Results in An Hour
Patients who go to a doctor for a blood test often have to contend with a needle and syringe, followed by a long wait—sometimes hours or even days—for lab results. Scientists have been working hard to... Read more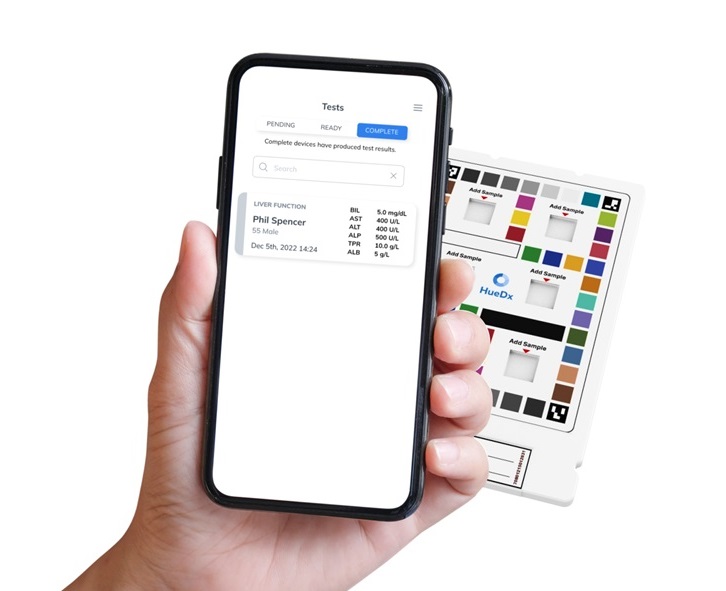
Smartphone-Enabled, Paper-Based Quantitative Diagnostic Platform Transforms POC Testing
Point-of-care diagnostics are crucial for public health, offering rapid, on-site testing that enables prompt diagnosis and treatment. This is especially valuable in remote or underserved regions where... Read moreBusiness
view channel
Hologic Acquires Gynesonics to Strengthen Existing Gynecological Surgical Business
Hologic (Marlborough, MA, USA) has signed a definitive agreement to acquire Gynesonics (Redwood City, CA, USA) for approximately USD 350 million, subject to working capital and other customary closing adjustments.... Read more