Inpatient Antibiotic Use in Hospitals Remains Unchanged
|
By HospiMedica International staff writers Posted on 26 Sep 2016 |
A new study warns that although the overall rate of antibiotic use in U.S. hospitalized patients has not changed significantly, increased prescription of broad-spectrum antibiotics could have a significant impact on antibiotic-resistant infections.
Researchers at the U.S Centers for Disease Control and Prevention (CDC, Atlanta, GA, USA) conducted a retrospective analysis of adult and pediatric in-patient antibiotic use data from 2006 to 2012 in approximately 300 acute care hospitals, which yielded 34 million discharges representing 166 million patient-days. The researchers then estimated the days of therapy (DOT) per 1,000 patient-days and the proportion of hospital discharges in which a patient received at least one dose of an antibiotic during hospital stay.
They then calculated measures of antibiotic usage stratified by antibiotic class, year, and other patient and facility characteristics, and created national estimates of antibiotic usage, also accounting for inter-hospital covariance to assess potential trends in antibiotic DOT over time. The results showed that 55.1% of patients received at least one dose of antibiotics during their hospital stay, with overall national DOTs at 755 per 1,000 patient-days.
While overall antibiotic use did not change significantly during the six-year time period, with total days of therapy increasing by just 5.6 days, the researchers noted that the use of several antibiotic classes, especially broad spectrum agents, increased significantly. These included tetracyclines, carbapenems, -lactam/-lactamase inhibitor combinations, glycopeptides, macrolides, and third- and fourth-generation cephalosporins. The study was published on September 19, 2016, in JAMA Internal Medicine.
“Owing to the rising threat of antibiotic resistance and other consequences resulting from unnecessary antibiotic use, ensuring appropriate antibiotic usage in the United States has become a national priority,” concluded lead author James Braggs, PhD, and colleagues. “The government has developed the National Strategy for Combating Antibiotic-Resistant Bacteria. Antibiotic use surveillance is a key objective within that strategy, and a core element of hospital antibiotic stewardship programs identified by the CDC. Appropriate antibiotic prescribing improves patient safety, slows development of antibiotic resistance, and reduces wasted resources.”
“We, as physicians, want to appear capable to our patients and not give the impression they have wasted either our time or their own,” wrote Ateev Mehrotra, MD, MPH, and Jeffrey Linder, MD, MPH, of Harvard Medical School (Boston, MA, USA), in an accompanying editorial. “In addition, it feels easier for us as physicians to do something now rather than wait for a problem to arise. In circumstances of diagnostic uncertainty, prescribing antibiotics ‘just to be safe’ feels like it decreases the chance of serious complications.”
Related Links:
U.S Centers for Disease Control and Prevention
Researchers at the U.S Centers for Disease Control and Prevention (CDC, Atlanta, GA, USA) conducted a retrospective analysis of adult and pediatric in-patient antibiotic use data from 2006 to 2012 in approximately 300 acute care hospitals, which yielded 34 million discharges representing 166 million patient-days. The researchers then estimated the days of therapy (DOT) per 1,000 patient-days and the proportion of hospital discharges in which a patient received at least one dose of an antibiotic during hospital stay.
They then calculated measures of antibiotic usage stratified by antibiotic class, year, and other patient and facility characteristics, and created national estimates of antibiotic usage, also accounting for inter-hospital covariance to assess potential trends in antibiotic DOT over time. The results showed that 55.1% of patients received at least one dose of antibiotics during their hospital stay, with overall national DOTs at 755 per 1,000 patient-days.
While overall antibiotic use did not change significantly during the six-year time period, with total days of therapy increasing by just 5.6 days, the researchers noted that the use of several antibiotic classes, especially broad spectrum agents, increased significantly. These included tetracyclines, carbapenems, -lactam/-lactamase inhibitor combinations, glycopeptides, macrolides, and third- and fourth-generation cephalosporins. The study was published on September 19, 2016, in JAMA Internal Medicine.
“Owing to the rising threat of antibiotic resistance and other consequences resulting from unnecessary antibiotic use, ensuring appropriate antibiotic usage in the United States has become a national priority,” concluded lead author James Braggs, PhD, and colleagues. “The government has developed the National Strategy for Combating Antibiotic-Resistant Bacteria. Antibiotic use surveillance is a key objective within that strategy, and a core element of hospital antibiotic stewardship programs identified by the CDC. Appropriate antibiotic prescribing improves patient safety, slows development of antibiotic resistance, and reduces wasted resources.”
“We, as physicians, want to appear capable to our patients and not give the impression they have wasted either our time or their own,” wrote Ateev Mehrotra, MD, MPH, and Jeffrey Linder, MD, MPH, of Harvard Medical School (Boston, MA, USA), in an accompanying editorial. “In addition, it feels easier for us as physicians to do something now rather than wait for a problem to arise. In circumstances of diagnostic uncertainty, prescribing antibiotics ‘just to be safe’ feels like it decreases the chance of serious complications.”
Related Links:
U.S Centers for Disease Control and Prevention
Latest Hospital News News
- Nurse Tracking System Improves Hospital Workflow
- New Children’s Hospital Transforms California Healthcare
- Noisy Hospitals Face Threat of Decreased Federal Compensation
- Orthopedics Centre of Excellence Planned for Guy’s Hospital
- Research Suggests Avoidance of Low-Value Surgical Procedures
- U.S. Federal Readmission Fines Linked to Higher Mortality
- Columbia China to Build New Hospital in Jiaxing
- Dubai Debuts Second Robotic Pharmacy Service
- Seattle Hospital Network Shifts Away from Overlapping Surgeries
- ACC to Launch Valvular Heart Disease Program in China
- Mortality Rates Lower at Major Teaching Hospitals
- South Australia to Inaugurate Upscale Hospital
- Raffles to Launch Second Hospital Project in China
- Research Center Tackles Antimicrobial Drugs Challenge
- Miami Cardiac & Vascular Institute Completes Expansion Project
- Hospital Antibiotic Policies Improve Prescription Practices
Channels
Critical Care
view channel
CPR Guidelines Updated for Pediatric and Neonatal Emergency Care and Resuscitation
Cardiac arrest in infants and children remains a leading cause of pediatric emergencies, with more than 7,000 out-of-hospital and 20,000 in-hospital cardiac arrests occurring annually in the United States.... Read more
Ingestible Capsule Monitors Intestinal Inflammation
Acute mesenteric ischemia—a life-threatening condition caused by blocked blood flow to the intestines—remains difficult to diagnose early because its symptoms often mimic common digestive problems.... Read more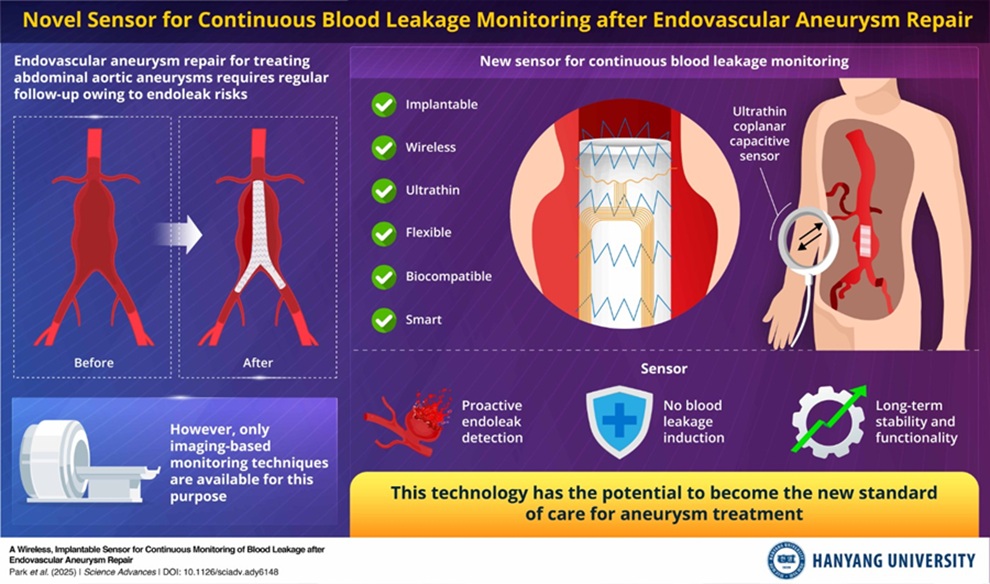
Wireless Implantable Sensor Enables Continuous Endoleak Monitoring
Endovascular aneurysm repair (EVAR) is a life-saving, minimally invasive treatment for abdominal aortic aneurysms—balloon-like bulges in the aorta that can rupture with fatal consequences.... Read more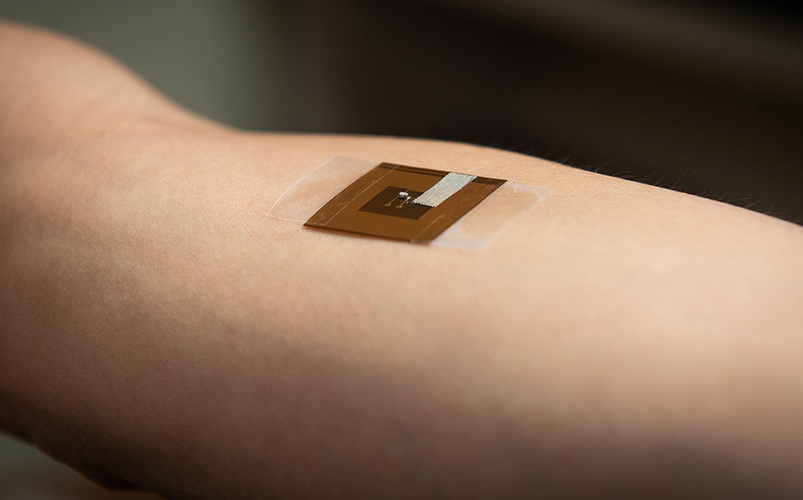
Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
Skin cancer remains one of the most dangerous and common cancers worldwide, with early detection crucial for improving survival rates. Traditional diagnostic methods—visual inspections, imaging, and biopsies—can... Read moreSurgical Techniques
view channel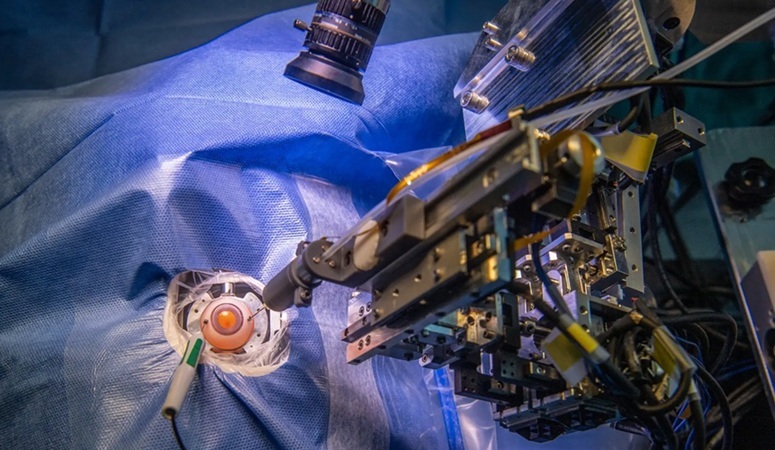
Robotic Assistant Delivers Ultra-Precision Injections with Rapid Setup Times
Age-related macular degeneration (AMD) is a leading cause of blindness worldwide, affecting nearly 200 million people, a figure expected to rise to 280 million by 2040. Current treatment involves doctors... Read more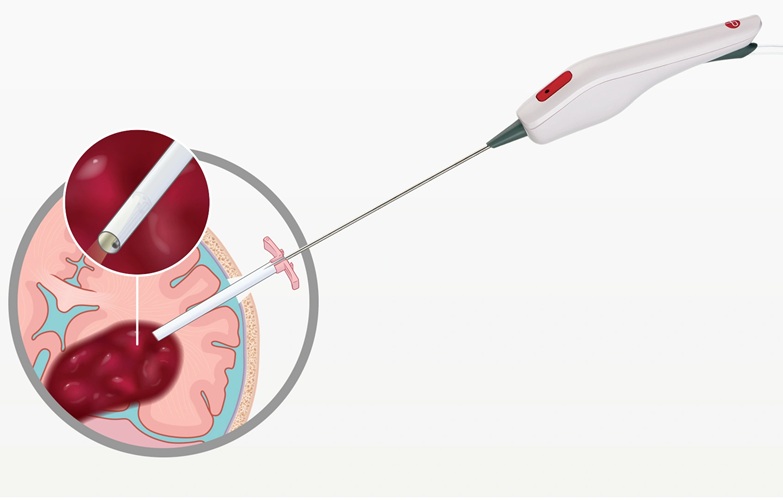
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more














