Hospital Antibiotic Policies Improve Prescription Practices
|
By HospiMedica International staff writers Posted on 21 Feb 2017 |
An updated review of studies identifies effective guidelines and policies to reduce unnecessary use of antibiotics in hospitals.
Researchers at the University of Dundee, University College London, and other institutions searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and Embase for studies examining the effectiveness and safety of interventions designed to improve antibiotic prescribing to hospital inpatients, and to investigate the effect of different intervention functions. In all, the researchers found 221 studies from the United States, Europe, Asia, South America, and Australia.
The researchers found that interventions broadly fell into two categories; 'restrictive' techniques applied rules to make physicians prescribe properly, whilst 'enabling' techniques provided advice or feedback to help physicians make more informed prescribing decisions. In both cases, the aim of the intervention was to increase the number of appropriate prescribing decisions so that patients who were unlikely to benefit from antibiotics did not get them, whilst they were still used for patients who stood to benefit from them.
The results showed that interventions that included enabling or restrictive techniques were consistently more effective than interventions that relied on simple education alone. Moreover, a synergistic effect existed, with enabling techniques increasing the effectiveness of restrictive techniques. In addition, the interventions shortened duration of antibiotic use from 11 to 9 days per patient, and reduced hospital stay from an average of 13 days to 12 per patient. The review was published on February 9, 2017, in The Cochrane Library.
“We do not need more studies to answer the question of whether these interventions reduce unnecessary antibiotic use, but we do need more research to understand why the most effective behavior change techniques are not more widely adopted within hospital settings,” concluded lead author Peter Davey, PhD, of the UD department of population health sciences. “Appropriate antibiotic use in hospitals should ensure effective treatment of patients with infection, and reduce unnecessary prescriptions.”
For the study, the researchers defined restriction as using rules to reduce the opportunity to engage in the target behavior, or increase the target behavior by reducing the opportunity to engage in competing behaviors. Enablement was defined as increasing the means and reducing the barriers in order to increase capability or opportunity.
Researchers at the University of Dundee, University College London, and other institutions searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and Embase for studies examining the effectiveness and safety of interventions designed to improve antibiotic prescribing to hospital inpatients, and to investigate the effect of different intervention functions. In all, the researchers found 221 studies from the United States, Europe, Asia, South America, and Australia.
The researchers found that interventions broadly fell into two categories; 'restrictive' techniques applied rules to make physicians prescribe properly, whilst 'enabling' techniques provided advice or feedback to help physicians make more informed prescribing decisions. In both cases, the aim of the intervention was to increase the number of appropriate prescribing decisions so that patients who were unlikely to benefit from antibiotics did not get them, whilst they were still used for patients who stood to benefit from them.
The results showed that interventions that included enabling or restrictive techniques were consistently more effective than interventions that relied on simple education alone. Moreover, a synergistic effect existed, with enabling techniques increasing the effectiveness of restrictive techniques. In addition, the interventions shortened duration of antibiotic use from 11 to 9 days per patient, and reduced hospital stay from an average of 13 days to 12 per patient. The review was published on February 9, 2017, in The Cochrane Library.
“We do not need more studies to answer the question of whether these interventions reduce unnecessary antibiotic use, but we do need more research to understand why the most effective behavior change techniques are not more widely adopted within hospital settings,” concluded lead author Peter Davey, PhD, of the UD department of population health sciences. “Appropriate antibiotic use in hospitals should ensure effective treatment of patients with infection, and reduce unnecessary prescriptions.”
For the study, the researchers defined restriction as using rules to reduce the opportunity to engage in the target behavior, or increase the target behavior by reducing the opportunity to engage in competing behaviors. Enablement was defined as increasing the means and reducing the barriers in order to increase capability or opportunity.
Latest Hospital News News
- Nurse Tracking System Improves Hospital Workflow
- New Children’s Hospital Transforms California Healthcare
- Noisy Hospitals Face Threat of Decreased Federal Compensation
- Orthopedics Centre of Excellence Planned for Guy’s Hospital
- Research Suggests Avoidance of Low-Value Surgical Procedures
- U.S. Federal Readmission Fines Linked to Higher Mortality
- Columbia China to Build New Hospital in Jiaxing
- Dubai Debuts Second Robotic Pharmacy Service
- Seattle Hospital Network Shifts Away from Overlapping Surgeries
- ACC to Launch Valvular Heart Disease Program in China
- Mortality Rates Lower at Major Teaching Hospitals
- South Australia to Inaugurate Upscale Hospital
- Raffles to Launch Second Hospital Project in China
- Research Center Tackles Antimicrobial Drugs Challenge
- Miami Cardiac & Vascular Institute Completes Expansion Project
- USC Virtual Care Clinic to Employ Avatar Doctors
Channels
Artificial Intelligence
view channel
AI Model Identifies Rare Endocrine Disorder from Hand Images
Acromegaly is a rare, intractable disease that typically begins in middle age and causes enlargement of the hands and feet, changes in facial appearance, and abnormal bone and organ growth.... Read moreCritical Care
view channel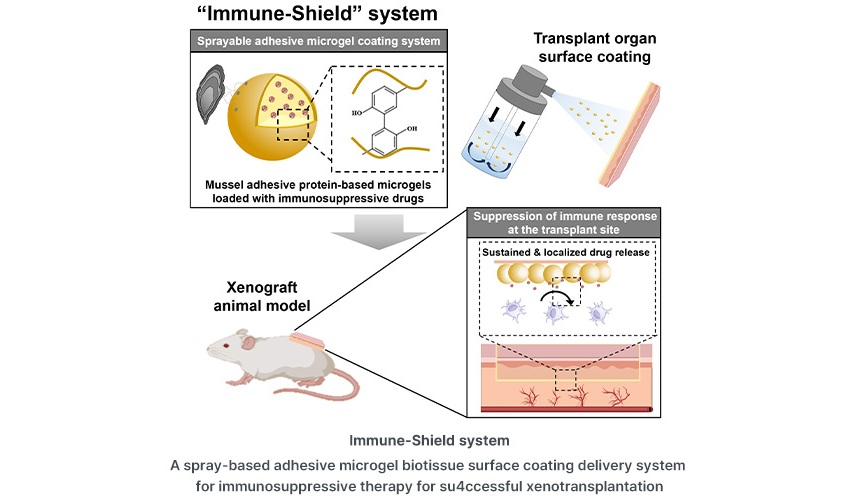
Spray-Type Technology Coats Transplant Organs with Immunosuppressants to Prevent Rejection
Organ transplantation is often the only life-saving option for patients with severe organ failure. However, immune rejection remains one of the biggest obstacles to successful transplantation.... Read more
Machine-Learning Model Predicts Preeclampsia in Late Pregnancy
Preeclampsia is a serious pregnancy complication marked by the sudden onset of high blood pressure before delivery. Affecting approximately 2% to 8% of pregnancies worldwide, the condition can lead to... Read more
Single Heart Attack Shot to Revolutionize Cardiac Care
Surviving a heart attack often marks the beginning of a long recovery period, during which the heart can remain vulnerable to damage and long-term weakening. Current treatments focus on stabilizing patients... Read more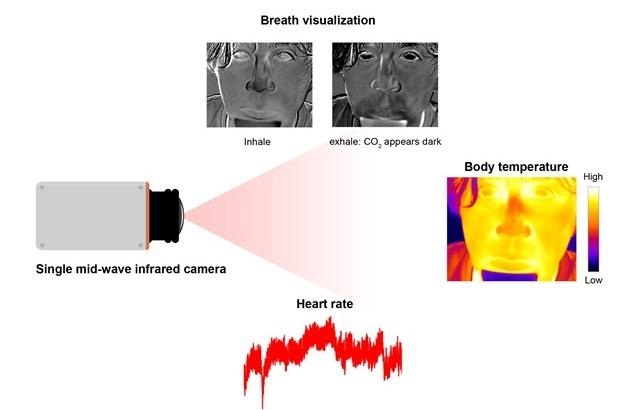
Single Mid-Wave Infrared Thermal Camera Enables Noncontact Vital Signs Monitoring
Infrared thermal cameras are widely used to measure surface temperatures and have become common tools for fever screening during infectious disease outbreaks. However, body temperature alone often provides... Read moreSurgical Techniques
view channel
Surgical Robot Makes Complex Liver Tumor Surgery Safer and Less Invasive
Tumors located in the caudate lobe of the liver present a major surgical challenge. This deep section of the liver sits close to critical blood vessels, making traditional surgical access difficult and... Read more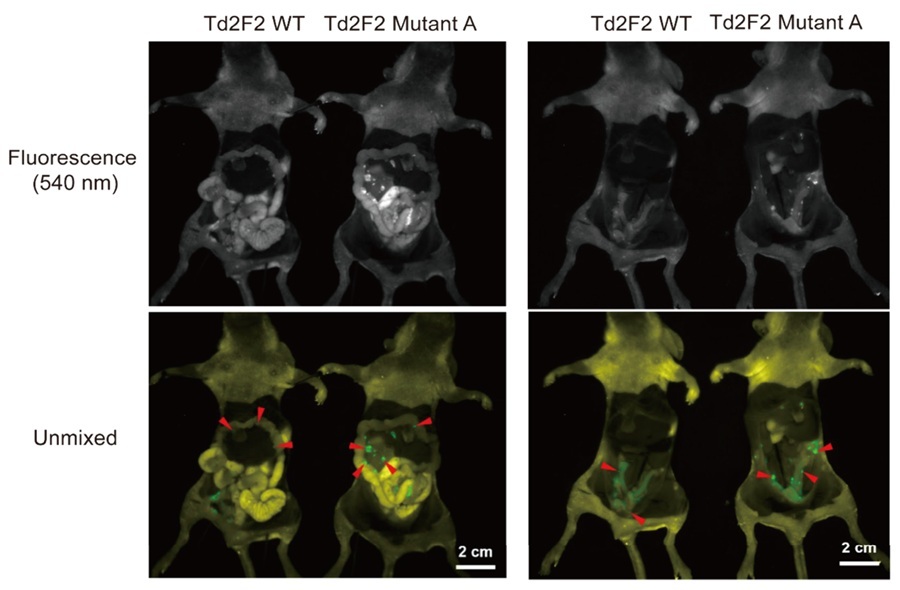
Fluorescence Probe Paired with Engineered Enzymes Lights Up Tumors for Easier Surgical Removal
Successful cancer surgery relies on a surgeon’s ability to remove tumors while preserving as much healthy tissue as possible. To assist with this, surgeons often use fluorescent dyes that cause cancer... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
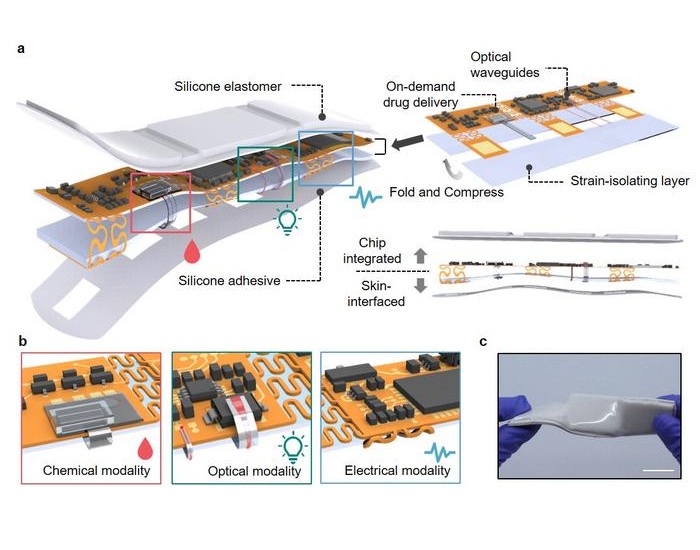
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more