Hand Hygiene Noncompliance and the Cost of Hospital-Acquired MRSA Infection
|
By HospiMedica International staff writers Posted on 21 Apr 2010 |
A new study shows that even minimal improvements in hand hygiene compliance is associated with significant and substantial savings in hospital costs.
Researchers at Duke University Medical Center (Durham, NC, USA) created two models to simulate sequential patient contacts by a hand hygiene-noncompliant healthcare worker. The first model involved encounters with patients of unknown methicillin-resistant Staphylococcus aureus (MRSA) status; the second model involved an encounter with an MRSA-colonized patient, followed by an encounter with a patient of unknown MRSA status. The probability of new MRSA infection for the second patient was then calculated using published data. In all, a simulation of one million noncompliant events was performed; the total costs of the resulting infections were then aggregated and amortized over all events. Estimates of MRSA prevalence, probability of transmission, and subsequent infection were derived from the published literature and experience at the study institution.
The results showed that the first model was associated with 42 MRSA infections, an infection rate of 0.0042%; the mean infection cost was US$47,092; and the mean cost per noncompliant event was $1.98. In the second model, noncompliance was associated with 980 MRSA infections, an infection rate of 0.098%; the mean infection cost was $53,598; the mean cost per noncompliant event was $52.53. Based on these figures, a 200-bed hospital incurs a total of $1,779,283 in annual MRSA infection-related expenses that are directly attributable to hand hygiene noncompliance. According to the researchers, a mere 1% increase in hand hygiene compliance would result in annual savings of $39,650; an increase in hand hygiene adherence by 5% would result in a mean decrease in expected MRSA-related costs of $198,250. The study was published in the April 2010 issue of Infection Control and Hospital Epidemiology.
"Many other pathogens are also spread to patients on the hands of healthcare workers as a result of noncompliance with hand hygiene. In fact, in some reports MRSA accounts for fewer than 8% of all hospital-acquired infections,” concluded lead author Keith Cummings, M.D., and colleagues of the department of medicine. "Because our model focused on costs associated only with MRSA transmission, it substantially underestimated the costs associated with hand hygiene noncompliance.”
Related Links:
Duke University Medical Center
Researchers at Duke University Medical Center (Durham, NC, USA) created two models to simulate sequential patient contacts by a hand hygiene-noncompliant healthcare worker. The first model involved encounters with patients of unknown methicillin-resistant Staphylococcus aureus (MRSA) status; the second model involved an encounter with an MRSA-colonized patient, followed by an encounter with a patient of unknown MRSA status. The probability of new MRSA infection for the second patient was then calculated using published data. In all, a simulation of one million noncompliant events was performed; the total costs of the resulting infections were then aggregated and amortized over all events. Estimates of MRSA prevalence, probability of transmission, and subsequent infection were derived from the published literature and experience at the study institution.
The results showed that the first model was associated with 42 MRSA infections, an infection rate of 0.0042%; the mean infection cost was US$47,092; and the mean cost per noncompliant event was $1.98. In the second model, noncompliance was associated with 980 MRSA infections, an infection rate of 0.098%; the mean infection cost was $53,598; the mean cost per noncompliant event was $52.53. Based on these figures, a 200-bed hospital incurs a total of $1,779,283 in annual MRSA infection-related expenses that are directly attributable to hand hygiene noncompliance. According to the researchers, a mere 1% increase in hand hygiene compliance would result in annual savings of $39,650; an increase in hand hygiene adherence by 5% would result in a mean decrease in expected MRSA-related costs of $198,250. The study was published in the April 2010 issue of Infection Control and Hospital Epidemiology.
"Many other pathogens are also spread to patients on the hands of healthcare workers as a result of noncompliance with hand hygiene. In fact, in some reports MRSA accounts for fewer than 8% of all hospital-acquired infections,” concluded lead author Keith Cummings, M.D., and colleagues of the department of medicine. "Because our model focused on costs associated only with MRSA transmission, it substantially underestimated the costs associated with hand hygiene noncompliance.”
Related Links:
Duke University Medical Center
Latest Critical Care News
- Machine Learning Tool Identifies Rare, Undiagnosed Immune Disorders from Patient EHRs
- On-Skin Wearable Bioelectronic Device Paves Way for Intelligent Implants
- First-Of-Its-Kind Dissolvable Stent to Improve Outcomes for Patients with Severe PAD
- AI Brain-Age Estimation Technology Uses EEG Scans to Screen for Degenerative Diseases
- Wheeze-Counting Wearable Device Monitors Patient's Breathing In Real Time
- Wearable Multiplex Biosensors Could Revolutionize COPD Management
- New Low-Energy Defibrillation Method Controls Cardiac Arrhythmias
- New Machine Learning Models Help Predict Heart Disease Risk in Women
- Deep-Learning Model Predicts Arrhythmia 30 Minutes before Onset
- Breakthrough Technology Combines Detection and Treatment of Nerve-Related Disorders in Single Procedure
- Plasma Irradiation Promotes Faster Bone Healing
- New Device Treats Acute Kidney Injury from Sepsis
- Study Confirms Safety of DCB-Only Strategy for Treating De Novo Left Main Coronary Artery Disease
- Revascularization Improves Quality of Life for Patients with Chronic Limb Threatening Ischemia
- AI-Driven Prediction Models Accurately Predict Critical Care Patient Deterioration
- Preventive PCI for High-Risk Coronary Plaques Reduces Cardiac Events
Channels
Artificial Intelligence
view channel
AI-Powered Algorithm to Revolutionize Detection of Atrial Fibrillation
Atrial fibrillation (AFib), a condition characterized by an irregular and often rapid heart rate, is linked to increased risks of stroke and heart failure. This is because the irregular heartbeat in AFib... Read more
AI Diagnostic Tool Accurately Detects Valvular Disorders Often Missed by Doctors
Doctors generally use stethoscopes to listen for the characteristic lub-dub sounds made by heart valves opening and closing. They also listen for less prominent sounds that indicate problems with these valves.... Read moreSurgical Techniques
view channel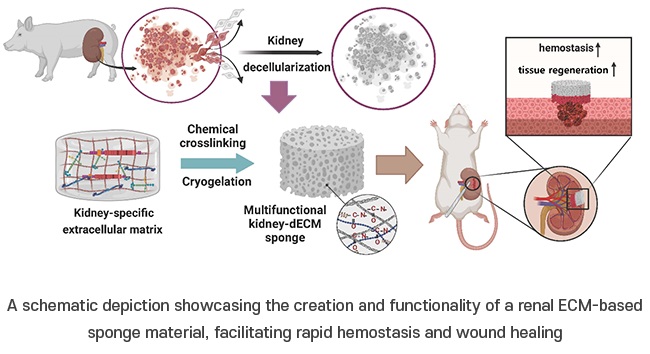
Porous Gel Sponge Facilitates Rapid Hemostasis and Wound Healing
The kidneys are essential organs that handle critical bodily functions, including waste elimination and blood pressure regulation. Often referred to as the silent organ because they typically do not manifest... Read more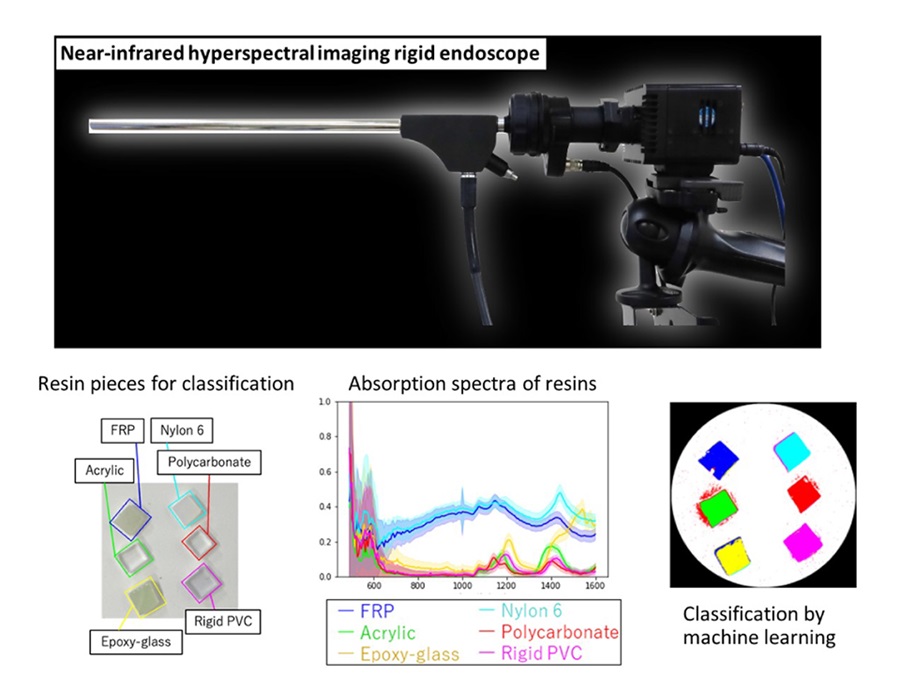
Novel Rigid Endoscope System Enables Deep Tissue Imaging During Surgery
Hyperspectral imaging (HSI) is an advanced technique that captures and processes information across a given electromagnetic spectrum. Near-infrared hyperspectral imaging (NIR-HSI) has particularly gained... Read more
Robotic Nerve ‘Cuffs’ Could Treat Various Neurological Conditions
Electric nerve implants serve dual functions: they can either stimulate or block signals in specific nerves. For example, they may alleviate pain by inhibiting pain signals or restore movement in paralyzed... Read more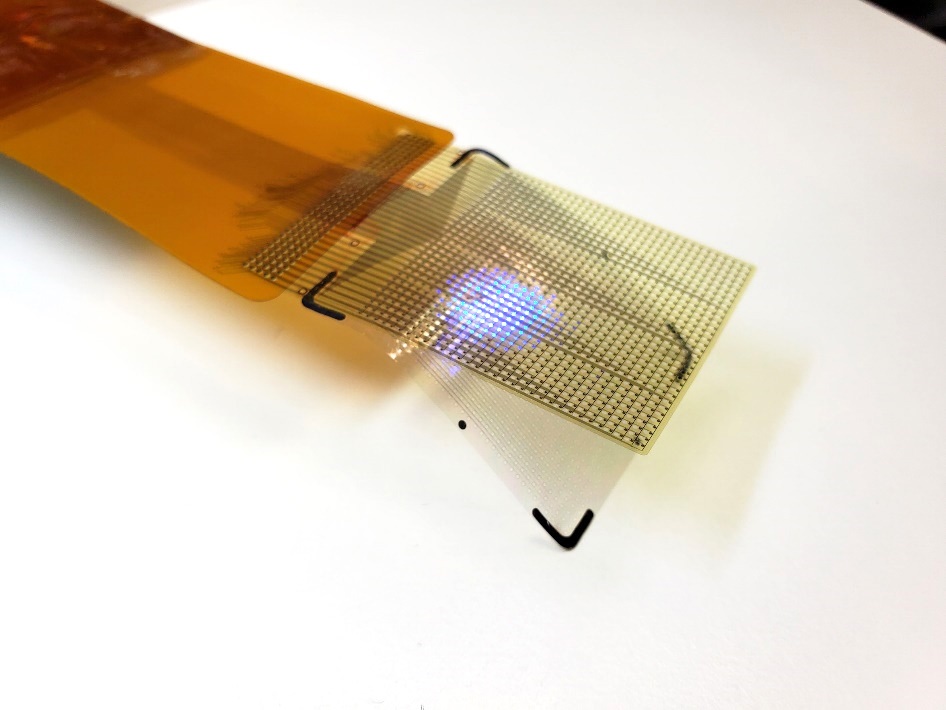
Flexible Microdisplay Visualizes Brain Activity in Real-Time To Guide Neurosurgeons
During brain surgery, neurosurgeons need to identify and preserve regions responsible for critical functions while removing harmful tissue. Traditionally, neurosurgeons rely on a team of electrophysiologists,... Read morePatient Care
view channelFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read more
Point of Care HIV Test Enables Early Infection Diagnosis for Infants
Early diagnosis and initiation of treatment are crucial for the survival of infants infected with HIV (human immunodeficiency virus). Without treatment, approximately 50% of infants who acquire HIV during... Read more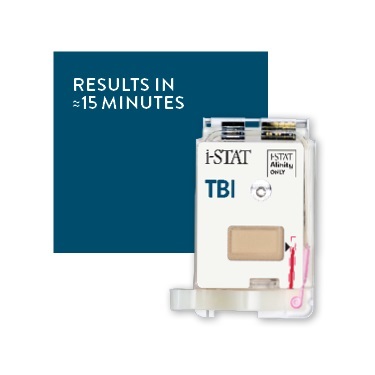
Whole Blood Rapid Test Aids Assessment of Concussion at Patient's Bedside
In the United States annually, approximately five million individuals seek emergency department care for traumatic brain injuries (TBIs), yet over half of those suspecting a concussion may never get it checked.... Read more
New Generation Glucose Hospital Meter System Ensures Accurate, Interference-Free and Safe Use
A new generation glucose hospital meter system now comes with several features that make hospital glucose testing easier and more secure while continuing to offer accuracy, freedom from interference, and... Read moreBusiness
view channel
Johnson & Johnson Acquires Cardiovascular Medical Device Company Shockwave Medical
Johnson & Johnson (New Brunswick, N.J., USA) and Shockwave Medical (Santa Clara, CA, USA) have entered into a definitive agreement under which Johnson & Johnson will acquire all of Shockwave’s... Read more