Medical Device Interoperability Could Improve Patient Care
|
By HospiMedica International staff writers Posted on 26 Apr 2015 |
Device interoperability, the ability to safely share health information across various technologies and systems, could enhanced patient safety and provide better clinical outcomes.
Researchers at the West Health Institute (WHI; La Jolla, CA, USA) conducted an online national survey of 526 nurses to study the impact of the current lack of interoperability among medical devices in the hospital setting on patient care. The devices in question included everything from infusion pumps, ventilators, pulse oximeters, and blood pressure cuffs to electronic health records (EHRs).
Among the nurses, 50% said they had witnessed a medical error due to lack of device coordination, and 60% said medical errors could be significantly reduced if medical devices were connected and shared data with each other automatically. Nearly half of these nurses (46%) claimed an error is extremely or very likely to occur when information must be manually transcribed from one device to another, with 69% adding that manually transcribing data is very likely to take time away from patients who need attention.
“Nurses are the front line of patient care and have an unrivaled ability to identify and address problems at the intersection of patients and technology,” said Joseph Smith, MD, chief medical and science officer at WHI. “The survey helps show how much of a nurse’s time could be better spent in direct care of patients and families, and how errors could be potentially avoided if medical devices, which have been so successful at improving patient care, were able to take the next step and seamlessly share critical information around the patient’s bedside.”
“Nurses enter the profession because they want to care for patients, not because they are interested in programming machines,” said Patricia Folcarelli, RN, of Beth Israel Deaconess Medical Center (Boston, MA, USA). “As many as 10 devices may monitor or treat a single patient in an intensive care unit. The nurse not only has to program and monitor the machines, he or she often spends a significant amount of time transcribing data by hand because the devices are not designed to share information.”
The researchers concluded that in order to make widespread medical device interoperability a reality, three key actions need to be taken:
Encourage the Office of the National Coordinator for Health Information Technology (ONC; Washington DC, USA) to specifically include the capture, integration, and sharing of medical device information in their nationwide interoperability roadmap.
Encourage the US Food and Drug Administration (FDA) and the US Department of Health & Human Services (HHS; Washington DC, USA) to recognize open standards for medical device communication and provide guidance for manufacturers regarding the design, testing and labeling of interoperable medical devices.
Ensure there are adequate incentives included in any Congressional legislation for the development and use of interoperable medical devices moving forward.
Related Links:
West Health Institute
US Department of Health & Human Services
Researchers at the West Health Institute (WHI; La Jolla, CA, USA) conducted an online national survey of 526 nurses to study the impact of the current lack of interoperability among medical devices in the hospital setting on patient care. The devices in question included everything from infusion pumps, ventilators, pulse oximeters, and blood pressure cuffs to electronic health records (EHRs).
Among the nurses, 50% said they had witnessed a medical error due to lack of device coordination, and 60% said medical errors could be significantly reduced if medical devices were connected and shared data with each other automatically. Nearly half of these nurses (46%) claimed an error is extremely or very likely to occur when information must be manually transcribed from one device to another, with 69% adding that manually transcribing data is very likely to take time away from patients who need attention.
“Nurses are the front line of patient care and have an unrivaled ability to identify and address problems at the intersection of patients and technology,” said Joseph Smith, MD, chief medical and science officer at WHI. “The survey helps show how much of a nurse’s time could be better spent in direct care of patients and families, and how errors could be potentially avoided if medical devices, which have been so successful at improving patient care, were able to take the next step and seamlessly share critical information around the patient’s bedside.”
“Nurses enter the profession because they want to care for patients, not because they are interested in programming machines,” said Patricia Folcarelli, RN, of Beth Israel Deaconess Medical Center (Boston, MA, USA). “As many as 10 devices may monitor or treat a single patient in an intensive care unit. The nurse not only has to program and monitor the machines, he or she often spends a significant amount of time transcribing data by hand because the devices are not designed to share information.”
The researchers concluded that in order to make widespread medical device interoperability a reality, three key actions need to be taken:
Encourage the Office of the National Coordinator for Health Information Technology (ONC; Washington DC, USA) to specifically include the capture, integration, and sharing of medical device information in their nationwide interoperability roadmap.
Encourage the US Food and Drug Administration (FDA) and the US Department of Health & Human Services (HHS; Washington DC, USA) to recognize open standards for medical device communication and provide guidance for manufacturers regarding the design, testing and labeling of interoperable medical devices.
Ensure there are adequate incentives included in any Congressional legislation for the development and use of interoperable medical devices moving forward.
Related Links:
West Health Institute
US Department of Health & Human Services
Latest Health IT News
- Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
- Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
- AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
- AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
- First Fully Autonomous Generative AI Personalized Medical Authorizations System Reduces Care Delay
- Electronic Health Records May Be Key to Improving Patient Care, Study Finds
- AI Trained for Specific Vocal Biomarkers Could Accurately Predict Coronary Artery Disease
- First-Ever AI Test for Early Diagnosis of Alzheimer’s to Be Expanded to Diagnosis of Parkinson’s Disease
- New Self-Learning AI-Based Algorithm Reads Electrocardiograms to Spot Unseen Signs of Heart Failure
- Autonomous Robot Performs COVID-19 Nasal Swab Tests

- Statistical Tool Predicts COVID-19 Peaks Worldwide
- Wireless-Controlled Soft Neural Implant Stimulates Brain Cells
- Tiny Polymer Stent Could Treat Pediatric Urethral Strictures
- Human Torso Simulator Helps Design Brace Innovations
- 3D Bioprinting Rebuilds the Human Heart
Channels
Artificial Intelligence
view channel
AI-Powered Algorithm to Revolutionize Detection of Atrial Fibrillation
Atrial fibrillation (AFib), a condition characterized by an irregular and often rapid heart rate, is linked to increased risks of stroke and heart failure. This is because the irregular heartbeat in AFib... Read more
AI Diagnostic Tool Accurately Detects Valvular Disorders Often Missed by Doctors
Doctors generally use stethoscopes to listen for the characteristic lub-dub sounds made by heart valves opening and closing. They also listen for less prominent sounds that indicate problems with these valves.... Read moreCritical Care
view channel
Powerful AI Risk Assessment Tool Predicts Outcomes in Heart Failure Patients
Heart failure is a serious condition where the heart cannot pump sufficient blood to meet the body's needs, leading to symptoms like fatigue, weakness, and swelling in the legs and feet, and it can ultimately... Read more
Peptide-Based Hydrogels Repair Damaged Organs and Tissues On-The-Spot
Scientists have ingeniously combined biomedical expertise with nature-inspired engineering to develop a jelly-like material that holds significant promise for immediate repairs to a wide variety of damaged... Read more
One-Hour Endoscopic Procedure Could Eliminate Need for Insulin for Type 2 Diabetes
Over 37 million Americans are diagnosed with diabetes, and more than 90% of these cases are Type 2 diabetes. This form of diabetes is most commonly seen in individuals over 45, though an increasing number... Read moreSurgical Techniques
view channel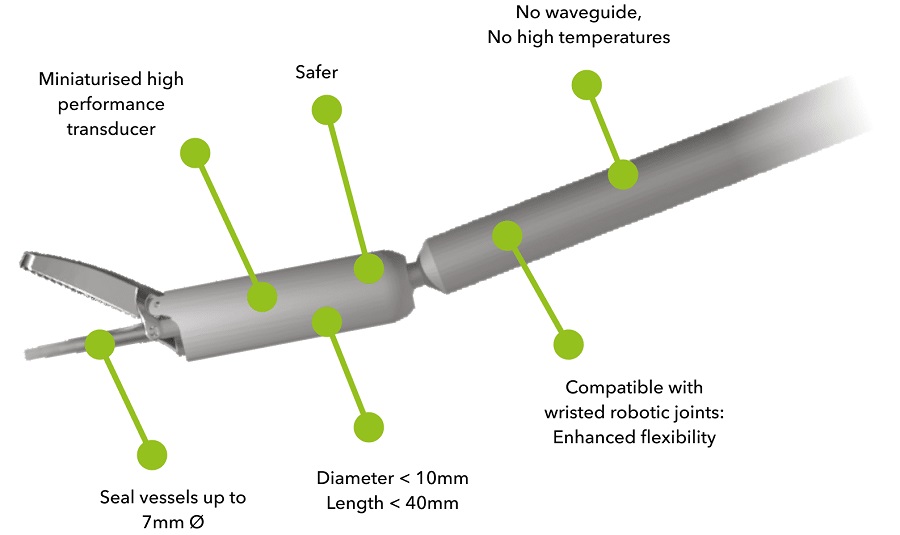
Miniaturized Ultrasonic Scalpel Enables Faster and Safer Robotic-Assisted Surgery
Robot-assisted surgery (RAS) has gained significant popularity in recent years and is now extensively used across various surgical fields such as urology, gynecology, and cardiology. These surgeries, performed... Read moreAI Assisted Reading Tool for Small Bowel Video Capsule Endoscopy Detects More Lesions
A revolutionary artificial intelligence (AI) technology that has proven faster and more accurate in diagnosing small bowel bleeding could transform gastrointestinal medicine. AnX Robotica (Plano, TX,... Read more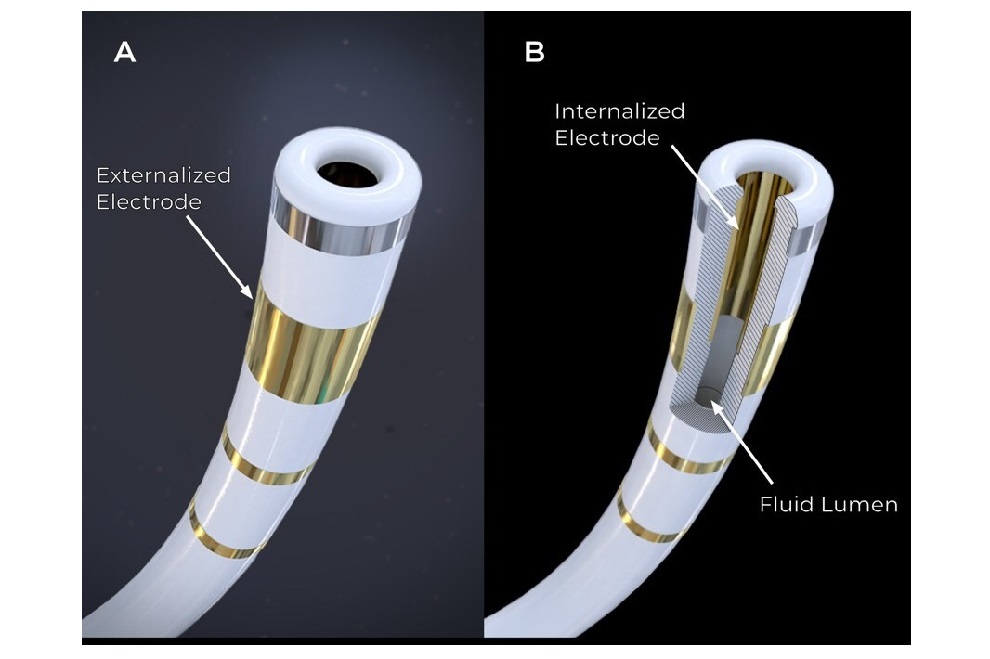
First-Ever Contact Force Pulsed Field Ablation System to Transform Treatment of Ventricular Arrhythmias
It is estimated that over 6 million patients in the US and Europe are affected by ventricular arrhythmias, which include conditions such as ventricular tachycardia (VT) and premature ventricular contractions (PVCs).... Read more
Caterpillar Robot with Built-In Steering System Crawls Easily Through Loops and Bends
Soft robots often face challenges in being guided effectively because adding steering mechanisms typically reduces their flexibility by increasing rigidity. Now, a team of engineers has combined ancient... Read morePatient Care
view channelFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read morePoint of Care
view channel
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read more
Point of Care HIV Test Enables Early Infection Diagnosis for Infants
Early diagnosis and initiation of treatment are crucial for the survival of infants infected with HIV (human immunodeficiency virus). Without treatment, approximately 50% of infants who acquire HIV during... Read more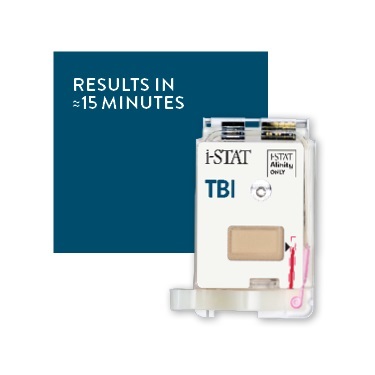
Whole Blood Rapid Test Aids Assessment of Concussion at Patient's Bedside
In the United States annually, approximately five million individuals seek emergency department care for traumatic brain injuries (TBIs), yet over half of those suspecting a concussion may never get it checked.... Read more
New Generation Glucose Hospital Meter System Ensures Accurate, Interference-Free and Safe Use
A new generation glucose hospital meter system now comes with several features that make hospital glucose testing easier and more secure while continuing to offer accuracy, freedom from interference, and... Read moreBusiness
view channel
Johnson & Johnson Acquires Cardiovascular Medical Device Company Shockwave Medical
Johnson & Johnson (New Brunswick, N.J., USA) and Shockwave Medical (Santa Clara, CA, USA) have entered into a definitive agreement under which Johnson & Johnson will acquire all of Shockwave’s... Read more