US Announces Agreement on Health Data Interoperability
|
By HospiMedica International staff writers Posted on 13 Mar 2016 |
The US Department of Health and Human Services (HHS; Washington DC, USA) has fostered an agreement on health data interoperability between providers and healthcare information technology (IT) firms.
More than a dozen leading professional associations and stakeholder groups pledged to implement three core commitments that will improve the flow of health information to consumers and healthcare providers. The first commitment is to help consumers easily and securely access their electronic health record (EHR) information, direct it to any desired location, learn how their information can be shared and used, and be assured that this information will be effectively and safely used to benefit their health and that of their community.
The second commitment is no information blocking by helping providers share personal EHR information with other providers and their patients whenever permitted by law, and not block EHR information, defined as knowingly and unreasonably interfering with information sharing.
The third commitment is to implement federally recognized, national interoperability standards, policies, guidance, and practices for electronic health information, and adopt best practices including those related to privacy and security. Many of the market leaders are embracing the Office of the National Coordinator for Health IT (ONC) Interoperability Standards Advisory, a coordinated catalog of existing and emerging standards and implementation specifications that is updated annually in order to keep pace with developments in the health IT industry.
“Today I am announcing that companies providing 90% of electronic health records used by hospitals have made a public commitment to make data work better for consumers and providers,” said Sylvia Burwell, secretary of the HHS, at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS). “Consumer access remains a challenge; it's great to have an electronic record, but if that record can't be easily accessed by doctors and patients because of funky technology, then we aren't consistently seeing the benefit.”
“We commend HHS for bringing so many stakeholders together, all of whom have an interest in using technology to result in a healthier and more efficient health care system,” said Steven Stack, MD, president of the American Medical Association (AMA; Chicago, IL, USA). “Patients and physicians are in this effort together because patients need easy access to their electronic health information, confident that it is secure and can be shared to benefit their health, and physicians need these electronic records to be interoperable to ensure that patients are receiving the best care possible.”
Many of the biggest health IT developers have already committed to using standardized application programming interfaces and Health Level 7 (HL7) fast health care interoperability resources (FHIR), so that user-friendly devices, such as smartphone and tablet apps, can quickly be made market-ready and compatible with one another. The use of a single shared standard for communicating among devices will make it easier for consumers to access their test results, track progress in their care, and communicate with their providers.
Related Links:
US Department of Health and Human Services
American Medical Association
More than a dozen leading professional associations and stakeholder groups pledged to implement three core commitments that will improve the flow of health information to consumers and healthcare providers. The first commitment is to help consumers easily and securely access their electronic health record (EHR) information, direct it to any desired location, learn how their information can be shared and used, and be assured that this information will be effectively and safely used to benefit their health and that of their community.
The second commitment is no information blocking by helping providers share personal EHR information with other providers and their patients whenever permitted by law, and not block EHR information, defined as knowingly and unreasonably interfering with information sharing.
The third commitment is to implement federally recognized, national interoperability standards, policies, guidance, and practices for electronic health information, and adopt best practices including those related to privacy and security. Many of the market leaders are embracing the Office of the National Coordinator for Health IT (ONC) Interoperability Standards Advisory, a coordinated catalog of existing and emerging standards and implementation specifications that is updated annually in order to keep pace with developments in the health IT industry.
“Today I am announcing that companies providing 90% of electronic health records used by hospitals have made a public commitment to make data work better for consumers and providers,” said Sylvia Burwell, secretary of the HHS, at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS). “Consumer access remains a challenge; it's great to have an electronic record, but if that record can't be easily accessed by doctors and patients because of funky technology, then we aren't consistently seeing the benefit.”
“We commend HHS for bringing so many stakeholders together, all of whom have an interest in using technology to result in a healthier and more efficient health care system,” said Steven Stack, MD, president of the American Medical Association (AMA; Chicago, IL, USA). “Patients and physicians are in this effort together because patients need easy access to their electronic health information, confident that it is secure and can be shared to benefit their health, and physicians need these electronic records to be interoperable to ensure that patients are receiving the best care possible.”
Many of the biggest health IT developers have already committed to using standardized application programming interfaces and Health Level 7 (HL7) fast health care interoperability resources (FHIR), so that user-friendly devices, such as smartphone and tablet apps, can quickly be made market-ready and compatible with one another. The use of a single shared standard for communicating among devices will make it easier for consumers to access their test results, track progress in their care, and communicate with their providers.
Related Links:
US Department of Health and Human Services
American Medical Association
Latest Health IT News
- Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
- Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
- AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
- AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
- First Fully Autonomous Generative AI Personalized Medical Authorizations System Reduces Care Delay
- Electronic Health Records May Be Key to Improving Patient Care, Study Finds
- AI Trained for Specific Vocal Biomarkers Could Accurately Predict Coronary Artery Disease
- First-Ever AI Test for Early Diagnosis of Alzheimer’s to Be Expanded to Diagnosis of Parkinson’s Disease
- New Self-Learning AI-Based Algorithm Reads Electrocardiograms to Spot Unseen Signs of Heart Failure
- Autonomous Robot Performs COVID-19 Nasal Swab Tests

- Statistical Tool Predicts COVID-19 Peaks Worldwide
- Wireless-Controlled Soft Neural Implant Stimulates Brain Cells
Channels
Critical Care
view channel_1.jpg)
Cutting-Edge Bioelectronic Device Offers Drug-Free Approach to Managing Bacterial Infections
Antibiotic-resistant infections pose an increasing threat to patient safety and healthcare systems worldwide. Recent estimates indicate that drug-resistant infections may rise by 70% by 2050, highlighting... Read more
Sophisticated Machine-Learning Approach Uses Patient EHRs to Predict Pneumonia Outcomes
Pneumonia, an infection that results in difficulty breathing due to fluid accumulation in the lungs, is one of the leading causes of death worldwide. This condition is particularly challenging to treat... Read more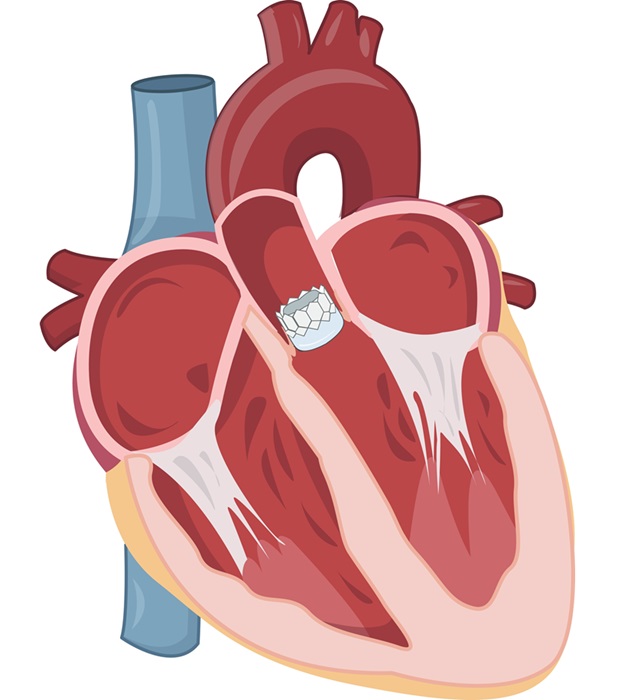
Early TAVR Benefits Patients with Asymptomatic Severe Aortic Stenosis
For patients with asymptomatic severe aortic stenosis (AS) and preserved left-ventricular ejection fraction, current guidelines recommend clinical surveillance every six to twelve months.... Read more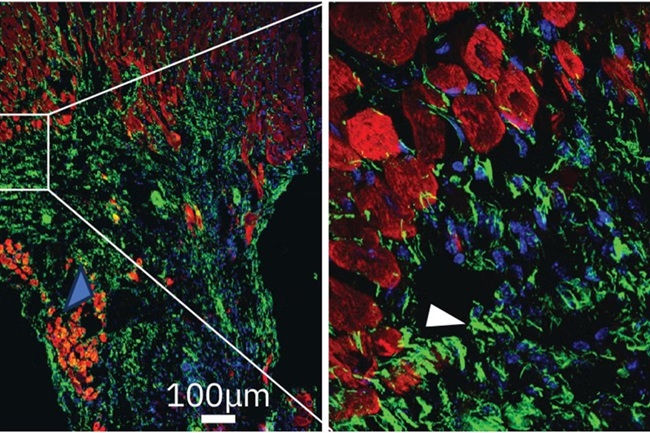
First-Of-Its-Kind Experimental Therapy Enhances Tissue Repair After Heart Attack
Cardiovascular disease remains the leading cause of death worldwide, accounting for one-third of all annual fatalities. Following a heart attack, the heart's natural regenerative ability is limited, resulting... Read moreSurgical Techniques
view channel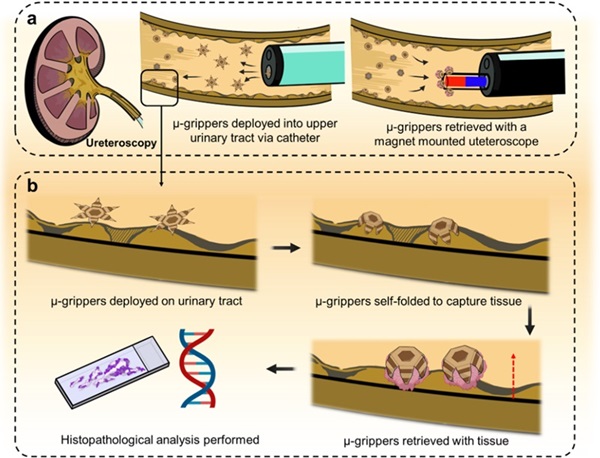
Microgrippers For Miniature Biopsies to Create New Cancer Diagnostic Screening Paradigm
The standard diagnosis of upper urinary tract cancers typically involves the removal of suspicious tissue using forceps, a procedure that is technically challenging and samples only a single region of the organ.... Read moreMiniature Soft Lithium-Ion Battery Could Be Used as Defibrillator During Surgery
The development of tiny smart devices, measuring just a few cubic millimeters, requires equally miniature power sources. For minimally invasive biomedical devices that interact with biological tissues,... Read more.jpg)
TAVI Procedure Supported by Radial Artery Access Reduces Bleeding Complications
The TAVI procedure, or Transcatheter Aortic Valve Implantation, is a minimally invasive technique in which a new aortic valve is inserted through a femoral artery to replace a narrowed old valve.... Read more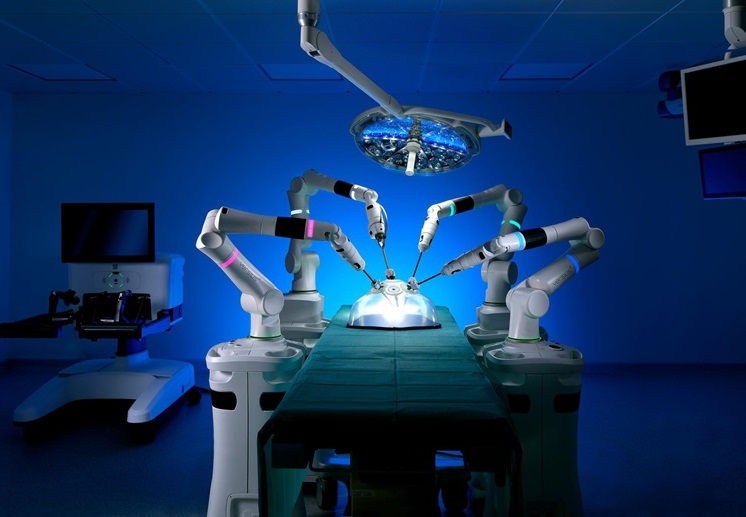
Portable Surgical Robot Seamlessly Integrates into Any OR for Performing Cholecystectomy Procedures
The United States represents a significant market with a strong demand for a flexible surgical robotic system applicable across various care settings. However, there has been a lack of sufficient options... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read morePoint of Care
view channel
Handheld, Sound-Based Diagnostic System Delivers Bedside Blood Test Results in An Hour
Patients who go to a doctor for a blood test often have to contend with a needle and syringe, followed by a long wait—sometimes hours or even days—for lab results. Scientists have been working hard to... Read more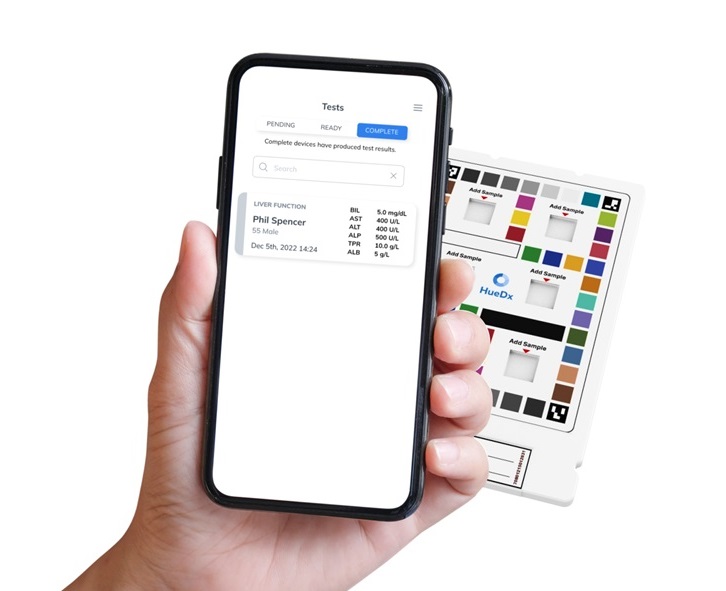
Smartphone-Enabled, Paper-Based Quantitative Diagnostic Platform Transforms POC Testing
Point-of-care diagnostics are crucial for public health, offering rapid, on-site testing that enables prompt diagnosis and treatment. This is especially valuable in remote or underserved regions where... Read moreBusiness
view channel
Hologic Acquires Gynesonics to Strengthen Existing Gynecological Surgical Business
Hologic (Marlborough, MA, USA) has signed a definitive agreement to acquire Gynesonics (Redwood City, CA, USA) for approximately USD 350 million, subject to working capital and other customary closing adjustments.... Read more