New Coating Reduces Catheter Pain and Infection Risk
|
By HospiMedica International staff writers Posted on 18 Mar 2020 |

Image: Dr. Nicola Irwin applying the coating to a catheter (Photo courtesy of QUB)
A new antimicrobial coating for urinary catheters and other medical devices can significantly reduce pain and risk of infection, according to a new study.
The coating, developed at Queen's University Belfast (QUB; United Kingdom) and the University of Leeds (United Kingdom), was created using a unique mix of polymers that reduce the coefficient of friction values in polyvinyl chloride (PVC) biomaterials by more than 300-fold, due to hydration of the surface-localized polymer network. To test the coating, the researchers created a clinically relevant model of the urinary tract in order to simulate the mechanical and biological environments encountered in vivo.
The researchers found that lubrication capacity was retained following hydration for periods lasting up to 28 days in artificial urine during 200 cycles of applied frictional force, both at a physiologically normal pH 6, and also at pH 9, which represents infected urine. The modified surfaces also demonstrated good antibacterial activity, achieving adherence reduction of 99.8% in common hospital-acquired pathogens, such as Staphylococcus aureus and Proteus mirabilis. The antibacterial activity was achieved by adding chlorhexidine into the coating matrix. The study was published on March 4, 2020, in ACS Applied Bio Materials.
“Patients with poor control over their bladder function, for example those with urinary retention or drainage problems caused by neurological conditions such as spina bifida or spinal cord injuries may need catheterization up to eight times a day,” said lead author Nicola Irwin, PhD, of QUB. “Insertion and removal of poorly lubricated catheters causes friction between the urethral walls and the device surface, which is not only extremely painful, but upon regular use can lead to damage and narrowing of the urethra, bleeding, and infection.”
“People who use medical devices such as catheters on a daily basis are at high risk of persistent low-level infections, which, overtime, can cause antibiotic resistance, one the biggest global threats to society today, leading to longer hospital stays, higher medical costs, and increased risk of infection and even death,” said study co-author Professor Colin McCoy, PhD, of QUB. “It is vitally important we provide an alternative to the currently used devices, which have not changed much since their introduction almost 100 years ago, despite their widespread clinical and many associated limitations.”
Related Links:
Queen's University Belfast
University of Leeds
The coating, developed at Queen's University Belfast (QUB; United Kingdom) and the University of Leeds (United Kingdom), was created using a unique mix of polymers that reduce the coefficient of friction values in polyvinyl chloride (PVC) biomaterials by more than 300-fold, due to hydration of the surface-localized polymer network. To test the coating, the researchers created a clinically relevant model of the urinary tract in order to simulate the mechanical and biological environments encountered in vivo.
The researchers found that lubrication capacity was retained following hydration for periods lasting up to 28 days in artificial urine during 200 cycles of applied frictional force, both at a physiologically normal pH 6, and also at pH 9, which represents infected urine. The modified surfaces also demonstrated good antibacterial activity, achieving adherence reduction of 99.8% in common hospital-acquired pathogens, such as Staphylococcus aureus and Proteus mirabilis. The antibacterial activity was achieved by adding chlorhexidine into the coating matrix. The study was published on March 4, 2020, in ACS Applied Bio Materials.
“Patients with poor control over their bladder function, for example those with urinary retention or drainage problems caused by neurological conditions such as spina bifida or spinal cord injuries may need catheterization up to eight times a day,” said lead author Nicola Irwin, PhD, of QUB. “Insertion and removal of poorly lubricated catheters causes friction between the urethral walls and the device surface, which is not only extremely painful, but upon regular use can lead to damage and narrowing of the urethra, bleeding, and infection.”
“People who use medical devices such as catheters on a daily basis are at high risk of persistent low-level infections, which, overtime, can cause antibiotic resistance, one the biggest global threats to society today, leading to longer hospital stays, higher medical costs, and increased risk of infection and even death,” said study co-author Professor Colin McCoy, PhD, of QUB. “It is vitally important we provide an alternative to the currently used devices, which have not changed much since their introduction almost 100 years ago, despite their widespread clinical and many associated limitations.”
Related Links:
Queen's University Belfast
University of Leeds
Latest Critical Care News
- Cutting-Edge Bioelectronic Device Offers Drug-Free Approach to Managing Bacterial Infections
- Early TAVR Benefits Patients with Asymptomatic Severe Aortic Stenosis
- Sophisticated Machine-Learning Approach Uses Patient EHRs to Predict Pneumonia Outcomes
- First-Of-Its-Kind Experimental Therapy Enhances Tissue Repair After Heart Attack
- AI Model Predicts Patients at Most Risk of Complication During Treatment for Advanced Kidney Failure
- AI Model Predicts Patients’ Risk of Developing and Worsening Disease from ECGs
- Grain-Sized Soft Robots Controlled by Magnetic Fields Deliver Medical Drugs

- AI Tool Helps Identify Heart Failure Risk in Diabetes Patients
- Inflammation Reducing Antibody Could Serve as Cardio-Immunotherapy for Heart Failure Patients
- AI Tool Accurately Identifies Patients Who Could Require Emergency Hospital Admission
- Simple Risk Score Model Helps Wean Patients from Mechanical Circulatory Support
- AI-Powered Wearable Camera System Detects Errors in Medication Delivery

- Re-Engineered Immune Cells Penetrate and Kill Solid Tumors
- New Nanoparticle Nanotherapy Infusion Cleans Arteries
- Fluorescence Imaging a Game-Changer for Bedside Biofilm Detection
- Spongelike Bandage with Antimicrobial Efficacy Stops Hemorrhaging and Mitigates Risk of Infection

Channels
Surgical Techniques
view channel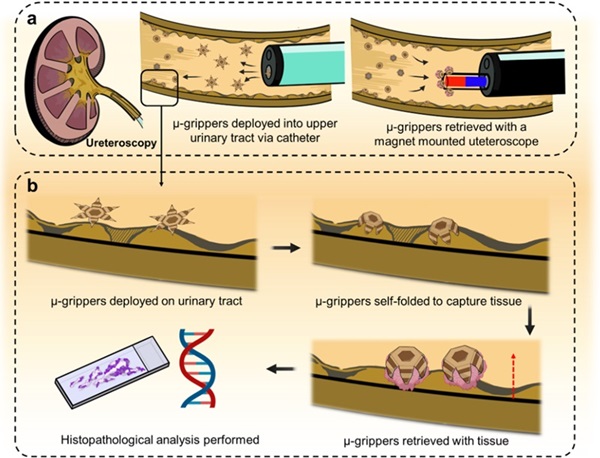
Microgrippers For Miniature Biopsies to Create New Cancer Diagnostic Screening Paradigm
The standard diagnosis of upper urinary tract cancers typically involves the removal of suspicious tissue using forceps, a procedure that is technically challenging and samples only a single region of the organ.... Read moreMiniature Soft Lithium-Ion Battery Could Be Used as Defibrillator During Surgery
The development of tiny smart devices, measuring just a few cubic millimeters, requires equally miniature power sources. For minimally invasive biomedical devices that interact with biological tissues,... Read more.jpg)
TAVI Procedure Supported by Radial Artery Access Reduces Bleeding Complications
The TAVI procedure, or Transcatheter Aortic Valve Implantation, is a minimally invasive technique in which a new aortic valve is inserted through a femoral artery to replace a narrowed old valve.... Read more
Portable Surgical Robot Seamlessly Integrates into Any OR for Performing Cholecystectomy Procedures
The United States represents a significant market with a strong demand for a flexible surgical robotic system applicable across various care settings. However, there has been a lack of sufficient options... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel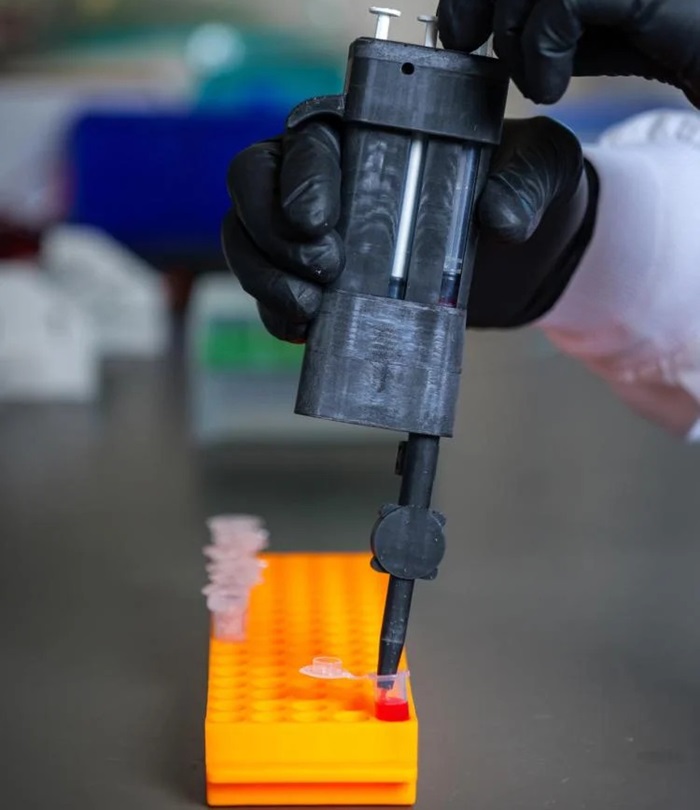
Handheld, Sound-Based Diagnostic System Delivers Bedside Blood Test Results in An Hour
Patients who go to a doctor for a blood test often have to contend with a needle and syringe, followed by a long wait—sometimes hours or even days—for lab results. Scientists have been working hard to... Read more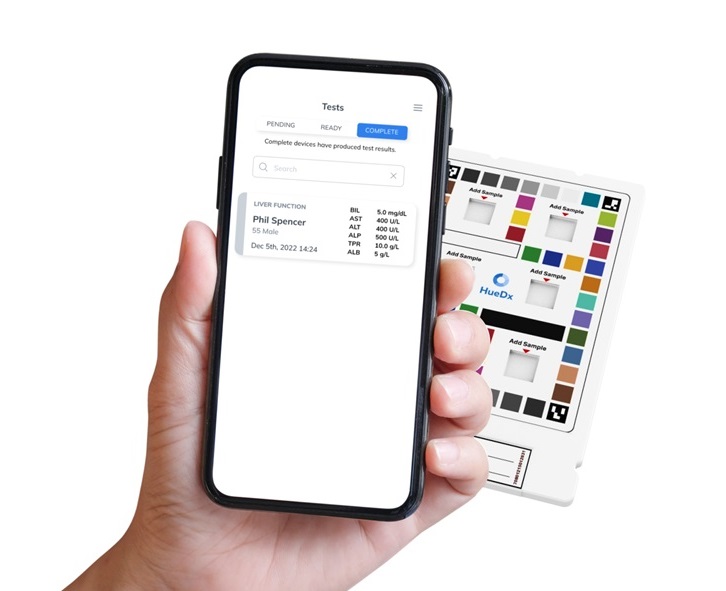
Smartphone-Enabled, Paper-Based Quantitative Diagnostic Platform Transforms POC Testing
Point-of-care diagnostics are crucial for public health, offering rapid, on-site testing that enables prompt diagnosis and treatment. This is especially valuable in remote or underserved regions where... Read moreBusiness
view channel
Hologic Acquires Gynesonics to Strengthen Existing Gynecological Surgical Business
Hologic (Marlborough, MA, USA) has signed a definitive agreement to acquire Gynesonics (Redwood City, CA, USA) for approximately USD 350 million, subject to working capital and other customary closing adjustments.... Read more