Front Line COVID-19 Critical Care Consortium Recommends Early Delivery of Anti-Inflammatory Therapies
|
By HospiMedica International staff writers Posted on 04 May 2020 |

Illustration
A group of five critical care specialists have jointly released a protocol for treating COVID-19 patients who are brought to hospitals, urging the immediate adoption of early intervention protocol to prevent mortality and reduce the need for ventilators.
The five leading critical care specialists, who together have formed the Front Line COVID-19 Critical Care Consortium, have released a protocol for treating patients who arrive in hospitals with COVID-19. Based on available research, the experience in China reflected by the Shanghai expert commission, and their decades-long professional experiences in Intensive Care Units (ICUs) around the country, the experts have strongly urged fellow physicians to immediately adopt a change in strategy by delivering powerful therapies earlier in the disease course, prior to admission to the ICU or the need for a mechanical ventilator. Based on early experiences with this more aggressive approach, they predict that early adoption of the protocol will reduce ICU admissions, obviate the need for mechanical ventilators, and most importantly, save many lives.
According to Dr. Pierre Kory, the Medical Director of the Trauma and Life Support Center and Chief of the Critical Care Service at the University of Wisconsin, it is the severe inflammation sparked by the coronavirus, not the virus itself that kills patients. Inflammation causes a new variety of Acute Respiratory Distress Syndrome (ARDS), which damages the lungs. The typical treatment for ARDS is to put patients on a mechanical ventilator, but Dr. Paul E. Marik, of the Eastern Virginia Medical School, says that should be the very last resort. The experts have emphasized that early intervention is critical in preventing the deterioration and death that has been described across the world once patients enter the ICU. By changing the therapeutic strategy towards initiating the combination of high-dose ascorbic acid and corticosteroids earlier in the disease course, the need for mechanical ventilation can be greatly reduced.
The critical care specialists have advised that in all COVID-19 hospitalized patients, the therapeutic focus must be placed on early intervention utilizing powerful, evidence-based therapies to counteract the overwhelming and damaging inflammatory response and the systemic and severe hyper-coagulable state causing organ damage By initiating the protocol within six hours of presentation in the emergency room, the need for mechanical ventilators and ICU beds will decrease dramatically, according to the experts.
“It is imperative that every hospital immediately adopt this safe, low-cost and highly effective treatment protocol, but they must implement it BEFORE the ICU, not after they reach the ICU because, in this disease, the organ damage tends to be so severe that patients rarely recover at that point,” said New York internist, Dr. Keith Berkowitz.
“This protocol will not only save patients’ lives, it will also lessen the danger to the doctors and nurses who treat them by decreasing the need for mechanical ventilators,” added Dr. Howard Kornfeld, President of the Pharmacology Policy Institute.
The five leading critical care specialists, who together have formed the Front Line COVID-19 Critical Care Consortium, have released a protocol for treating patients who arrive in hospitals with COVID-19. Based on available research, the experience in China reflected by the Shanghai expert commission, and their decades-long professional experiences in Intensive Care Units (ICUs) around the country, the experts have strongly urged fellow physicians to immediately adopt a change in strategy by delivering powerful therapies earlier in the disease course, prior to admission to the ICU or the need for a mechanical ventilator. Based on early experiences with this more aggressive approach, they predict that early adoption of the protocol will reduce ICU admissions, obviate the need for mechanical ventilators, and most importantly, save many lives.
According to Dr. Pierre Kory, the Medical Director of the Trauma and Life Support Center and Chief of the Critical Care Service at the University of Wisconsin, it is the severe inflammation sparked by the coronavirus, not the virus itself that kills patients. Inflammation causes a new variety of Acute Respiratory Distress Syndrome (ARDS), which damages the lungs. The typical treatment for ARDS is to put patients on a mechanical ventilator, but Dr. Paul E. Marik, of the Eastern Virginia Medical School, says that should be the very last resort. The experts have emphasized that early intervention is critical in preventing the deterioration and death that has been described across the world once patients enter the ICU. By changing the therapeutic strategy towards initiating the combination of high-dose ascorbic acid and corticosteroids earlier in the disease course, the need for mechanical ventilation can be greatly reduced.
The critical care specialists have advised that in all COVID-19 hospitalized patients, the therapeutic focus must be placed on early intervention utilizing powerful, evidence-based therapies to counteract the overwhelming and damaging inflammatory response and the systemic and severe hyper-coagulable state causing organ damage By initiating the protocol within six hours of presentation in the emergency room, the need for mechanical ventilators and ICU beds will decrease dramatically, according to the experts.
“It is imperative that every hospital immediately adopt this safe, low-cost and highly effective treatment protocol, but they must implement it BEFORE the ICU, not after they reach the ICU because, in this disease, the organ damage tends to be so severe that patients rarely recover at that point,” said New York internist, Dr. Keith Berkowitz.
“This protocol will not only save patients’ lives, it will also lessen the danger to the doctors and nurses who treat them by decreasing the need for mechanical ventilators,” added Dr. Howard Kornfeld, President of the Pharmacology Policy Institute.
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
Intestinal gases are associated with several health conditions, including colon cancer, irritable bowel syndrome, and inflammatory bowel disease, and they have the potential to serve as crucial biomarkers... Read moreNovel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
Multiphoton microscopy has become an invaluable tool in neuroscience, allowing researchers to observe brain activity in real time with high-resolution imaging. A crucial aspect of many multiphoton microscopy... Read more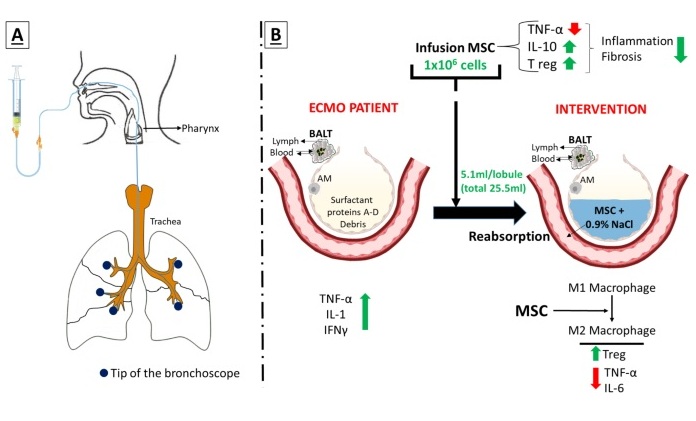
Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
Until now, administering cell therapies to patients on extracorporeal membrane oxygenation (ECMO)—a life-support system typically used for severe lung failure—has been nearly impossible.... Read moreSurgical Techniques
view channel
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more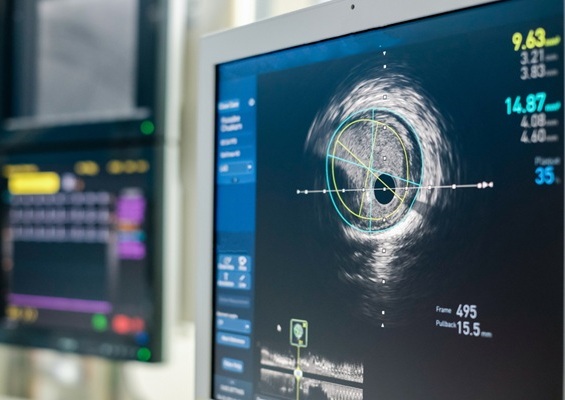
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more