COVID-19 Neurological Complications Could Cause Long Term Brain Damage in Recovered Patients, Warn Researchers
|
By HospiMedica International staff writers Posted on 14 Jul 2020 |
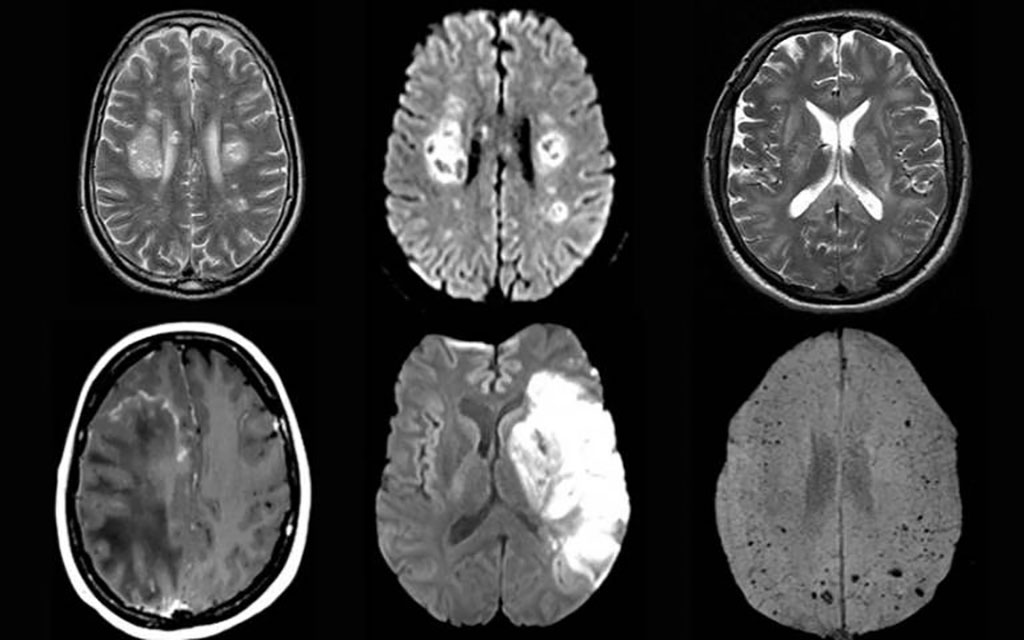
Image: Brain scan images from the study (Photo courtesy of University College London)
Researchers have warned that COVID-19 neurological complications, including delirium, brain inflammation, stroke, and nerve damage, could result in large scale brain damage in recovered patients over the long term.
In a new study by the University College London (London, UK), the research team identified one rare and sometimes fatal inflammatory condition, known as acute disseminated encephalomyelitis (ADEM), which appears to be increasing in prevalence due to the pandemic. Some patients in the study did not experience severe respiratory symptoms, and the neurological disorder was the first and main presentation of COVID-19.
The study provides a detailed account of neurological symptoms of 43 people who had either confirmed or suspected COVID-19. The researchers identified 10 cases of transient encephalopathies (temporary brain dysfunction) with delirium, which corresponds with other studies finding evidence of delirium with agitation. There were also 12 cases of brain inflammation, eight cases of strokes, and eight others with nerve damage, mainly Guillain-Barré syndrome (which usually occurs after a respiratory or gastrointestinal infection). Most (nine out of 12 cases) of those with brain inflammation conditions were diagnosed with ADEM, which is rare and typically seen in children and can be triggered by viral infections. The researchers normally see about one adult patient with ADEM per month, but that increased to at least one per week during the study period, which they said was a concerning increase.
SARS-CoV-2 was not detected in the cerebrospinal brain fluid of any of the patients tested, suggesting the virus did not directly attack the brain to cause the neurological illness. Further research is needed to identify why patients were developing these complications. In some patients, the researchers found evidence that the brain inflammation was likely caused by an immune response to the disease, suggesting that some neurological complications of COVID-19 might come from the immune response rather than the virus itself. The findings add clinical descriptions and detail to another recent study identifying 153 people with neurological complications from COVID-19. The latest study also confirmed the previously reported findings of a higher than expected number of patients with stroke resulting from excessive stickiness of blood in COVID-19 patients.
“We identified a higher than expected number of people with neurological conditions such as brain inflammation, which did not always correlate with the severity of respiratory symptoms,” said joint senior author Dr. Michael Zandi (UCL Queen Square Institute of Neurology and University College London Hospitals NHS Foundation Trust). “We should be vigilant and look out for these complications in people who have had COVID-19. Whether we will see an epidemic on a large scale of brain damage linked to the pandemic, perhaps similar to the encephalitis lethargica outbreak in the 1920s and 1930s after the 1918 influenza pandemic, remains to be seen.”
“Given that the disease has only been around for a matter of months, we might not yet know what long-term damage COVID-19 can cause,” said joint first author Dr. Ross Paterson from the UCL Queen Square Institute of Neurology. “Doctors need to be aware of possible neurological effects, as early diagnosis can improve patient outcomes. People recovering from the virus should seek professional health advice if they experience neurological symptoms.”
Related Links:
University College London
In a new study by the University College London (London, UK), the research team identified one rare and sometimes fatal inflammatory condition, known as acute disseminated encephalomyelitis (ADEM), which appears to be increasing in prevalence due to the pandemic. Some patients in the study did not experience severe respiratory symptoms, and the neurological disorder was the first and main presentation of COVID-19.
The study provides a detailed account of neurological symptoms of 43 people who had either confirmed or suspected COVID-19. The researchers identified 10 cases of transient encephalopathies (temporary brain dysfunction) with delirium, which corresponds with other studies finding evidence of delirium with agitation. There were also 12 cases of brain inflammation, eight cases of strokes, and eight others with nerve damage, mainly Guillain-Barré syndrome (which usually occurs after a respiratory or gastrointestinal infection). Most (nine out of 12 cases) of those with brain inflammation conditions were diagnosed with ADEM, which is rare and typically seen in children and can be triggered by viral infections. The researchers normally see about one adult patient with ADEM per month, but that increased to at least one per week during the study period, which they said was a concerning increase.
SARS-CoV-2 was not detected in the cerebrospinal brain fluid of any of the patients tested, suggesting the virus did not directly attack the brain to cause the neurological illness. Further research is needed to identify why patients were developing these complications. In some patients, the researchers found evidence that the brain inflammation was likely caused by an immune response to the disease, suggesting that some neurological complications of COVID-19 might come from the immune response rather than the virus itself. The findings add clinical descriptions and detail to another recent study identifying 153 people with neurological complications from COVID-19. The latest study also confirmed the previously reported findings of a higher than expected number of patients with stroke resulting from excessive stickiness of blood in COVID-19 patients.
“We identified a higher than expected number of people with neurological conditions such as brain inflammation, which did not always correlate with the severity of respiratory symptoms,” said joint senior author Dr. Michael Zandi (UCL Queen Square Institute of Neurology and University College London Hospitals NHS Foundation Trust). “We should be vigilant and look out for these complications in people who have had COVID-19. Whether we will see an epidemic on a large scale of brain damage linked to the pandemic, perhaps similar to the encephalitis lethargica outbreak in the 1920s and 1930s after the 1918 influenza pandemic, remains to be seen.”
“Given that the disease has only been around for a matter of months, we might not yet know what long-term damage COVID-19 can cause,” said joint first author Dr. Ross Paterson from the UCL Queen Square Institute of Neurology. “Doctors need to be aware of possible neurological effects, as early diagnosis can improve patient outcomes. People recovering from the virus should seek professional health advice if they experience neurological symptoms.”
Related Links:
University College London
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read more
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read moreSurgical Techniques
view channel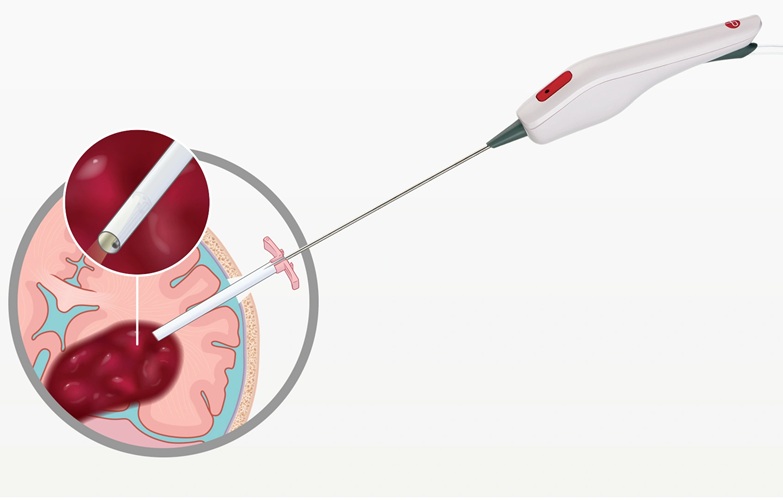
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read more
Novel Glue Prevents Complications After Breast Cancer Surgery
Seroma and prolonged lymphorrhea are among the most common complications following axillary lymphadenectomy in breast cancer patients. These postoperative issues can delay recovery and postpone the start... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more