Scientists Use Machine Learning Algorithm to Identify Six Types of COVID-19 with Distinctive Symptoms
|
By HospiMedica International staff writers Posted on 20 Jul 2020 |
Image: SARS-CoV-2 (Photo courtesy of NIAID)
An analysis of data from the COVID Symptom Study app has revealed that there are six distinct ‘types’ of COVID-19, each distinguished by a particular cluster of symptoms and differing in the severity of the disease as well as need for respiratory support during hospitalization.
The findings have major implications for clinical management of COVID-19, and could help doctors predict who is most at risk and likely to need hospital care in a second wave of coronavirus infections. Although continuous cough, fever and loss of smell (anosmia) are usually highlighted as the three key symptoms of COVID-19, data gathered from app users shows that people can experience a wide range of different symptoms including headaches, muscle pains, fatigue, diarrhea, confusion, loss of appetite, shortness of breath and more. The progression and outcomes also vary significantly between people, ranging from mild flu-like symptoms or a simple rash to severe or fatal disease.
To find out whether particular symptoms tend to appear together and how this related to the progression of the disease, the research team at King’s College London (London, UK) used a machine learning algorithm to analyze data from a subset of around 1,600 users in the UK and US with confirmed COVID-19 who had regularly logged their symptoms using the app in March and April. The analysis revealed six specific groupings of symptoms emerging at characteristic timepoints in the progression of the illness, representing six distinct ‘types’ of COVID-19. The algorithm was then tested by running it on a second independent dataset of 1,000 users in the UK, US and Sweden, who had logged their symptoms during May. All people reporting symptoms experienced headache and loss of smell, with varying combinations of additional symptoms at various times. Some of these, such as confusion, abdominal pain and shortness of breath, are not widely known as COVID-19 symptoms, yet are hallmarks of the most severe forms of the disease.
The team also discovered that people experiencing particular symptom clusters were more likely to require breathing support in the form of ventilation or additional oxygen. The researchers then developed a model combining information about age, sex, BMI and pre-existing conditions together with symptoms gathered over just five days from the onset of the illness. This was able to predict which cluster a patient falls into and their risk of requiring hospitalization and breathing support with a higher likelihood of being correct than an existing risk model based purely on age, sex, BMI and pre-existing conditions alone. Given that most people who require breathing support come to hospital around 13 days after their first symptoms, this extra eight days represents a significant ‘early warning’ as to who is most likely to need more intensive care.
“These findings have important implications for care and monitoring of people who are most vulnerable to severe COVID-19,” said Dr Claire Steves from King’s College London. “If you can predict who these people are at day five, you have time to give them support and early interventions such as monitoring blood oxygen and sugar levels, and ensuring they are properly hydrated - simple care that could be given at home, preventing hospitalizations and saving lives.”
“Being able to gather big datasets through the app and apply machine learning to them is having a profound impact on our understanding of the extent and impact of COVID-19, and human health more widely,” said Sebastien Ourselin, professor of healthcare engineering at King’s College London and senior author of the study.
Related Links:
King’s College London
The findings have major implications for clinical management of COVID-19, and could help doctors predict who is most at risk and likely to need hospital care in a second wave of coronavirus infections. Although continuous cough, fever and loss of smell (anosmia) are usually highlighted as the three key symptoms of COVID-19, data gathered from app users shows that people can experience a wide range of different symptoms including headaches, muscle pains, fatigue, diarrhea, confusion, loss of appetite, shortness of breath and more. The progression and outcomes also vary significantly between people, ranging from mild flu-like symptoms or a simple rash to severe or fatal disease.
To find out whether particular symptoms tend to appear together and how this related to the progression of the disease, the research team at King’s College London (London, UK) used a machine learning algorithm to analyze data from a subset of around 1,600 users in the UK and US with confirmed COVID-19 who had regularly logged their symptoms using the app in March and April. The analysis revealed six specific groupings of symptoms emerging at characteristic timepoints in the progression of the illness, representing six distinct ‘types’ of COVID-19. The algorithm was then tested by running it on a second independent dataset of 1,000 users in the UK, US and Sweden, who had logged their symptoms during May. All people reporting symptoms experienced headache and loss of smell, with varying combinations of additional symptoms at various times. Some of these, such as confusion, abdominal pain and shortness of breath, are not widely known as COVID-19 symptoms, yet are hallmarks of the most severe forms of the disease.
The team also discovered that people experiencing particular symptom clusters were more likely to require breathing support in the form of ventilation or additional oxygen. The researchers then developed a model combining information about age, sex, BMI and pre-existing conditions together with symptoms gathered over just five days from the onset of the illness. This was able to predict which cluster a patient falls into and their risk of requiring hospitalization and breathing support with a higher likelihood of being correct than an existing risk model based purely on age, sex, BMI and pre-existing conditions alone. Given that most people who require breathing support come to hospital around 13 days after their first symptoms, this extra eight days represents a significant ‘early warning’ as to who is most likely to need more intensive care.
“These findings have important implications for care and monitoring of people who are most vulnerable to severe COVID-19,” said Dr Claire Steves from King’s College London. “If you can predict who these people are at day five, you have time to give them support and early interventions such as monitoring blood oxygen and sugar levels, and ensuring they are properly hydrated - simple care that could be given at home, preventing hospitalizations and saving lives.”
“Being able to gather big datasets through the app and apply machine learning to them is having a profound impact on our understanding of the extent and impact of COVID-19, and human health more widely,” said Sebastien Ourselin, professor of healthcare engineering at King’s College London and senior author of the study.
Related Links:
King’s College London
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
CPR Guidelines Updated for Pediatric and Neonatal Emergency Care and Resuscitation
Cardiac arrest in infants and children remains a leading cause of pediatric emergencies, with more than 7,000 out-of-hospital and 20,000 in-hospital cardiac arrests occurring annually in the United States.... Read more
Ingestible Capsule Monitors Intestinal Inflammation
Acute mesenteric ischemia—a life-threatening condition caused by blocked blood flow to the intestines—remains difficult to diagnose early because its symptoms often mimic common digestive problems.... Read more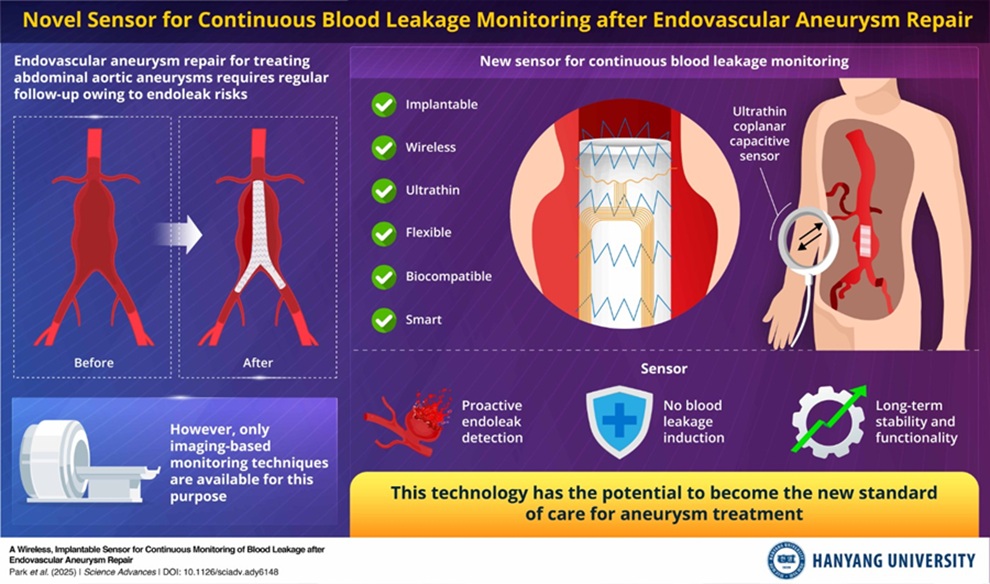
Wireless Implantable Sensor Enables Continuous Endoleak Monitoring
Endovascular aneurysm repair (EVAR) is a life-saving, minimally invasive treatment for abdominal aortic aneurysms—balloon-like bulges in the aorta that can rupture with fatal consequences.... Read more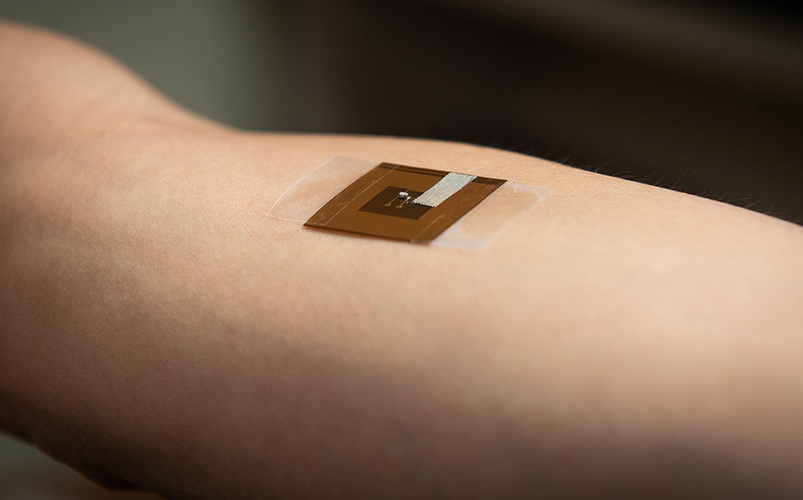
Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
Skin cancer remains one of the most dangerous and common cancers worldwide, with early detection crucial for improving survival rates. Traditional diagnostic methods—visual inspections, imaging, and biopsies—can... Read moreSurgical Techniques
view channel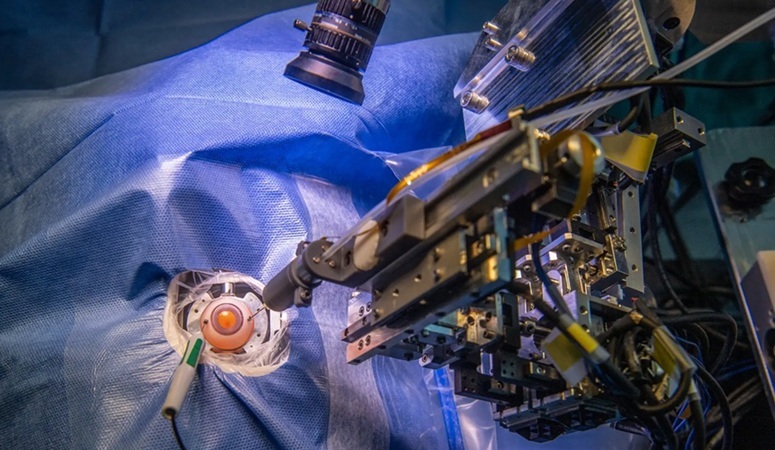
Robotic Assistant Delivers Ultra-Precision Injections with Rapid Setup Times
Age-related macular degeneration (AMD) is a leading cause of blindness worldwide, affecting nearly 200 million people, a figure expected to rise to 280 million by 2040. Current treatment involves doctors... Read more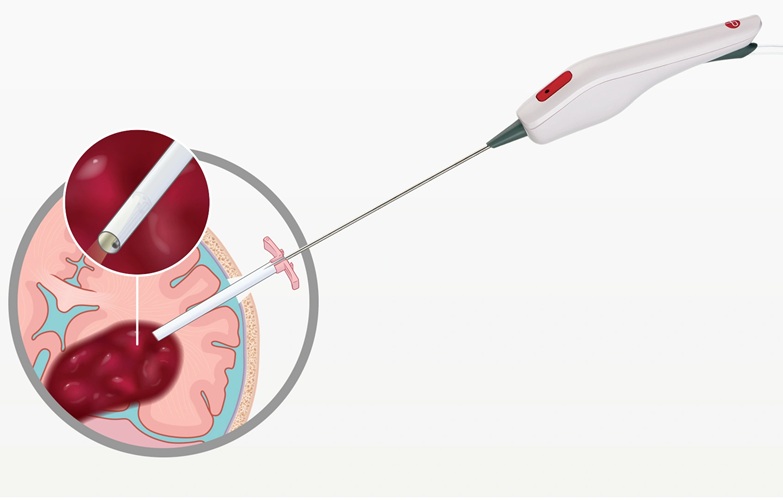
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more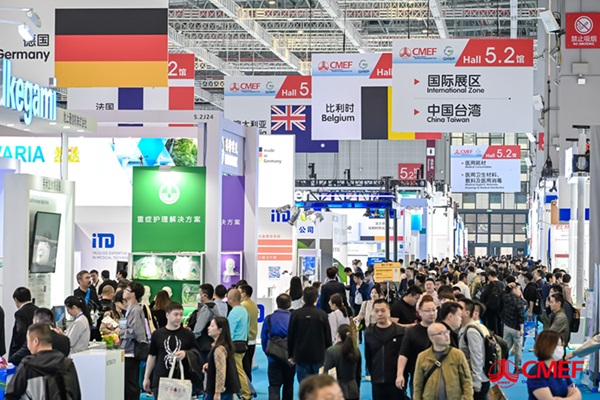
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more