COVID-19 Mathematical Model Indicates Flu Season May Cause 2.5-Fold Increase in Coronavirus Transmission
|
By HospiMedica International staff writers Posted on 16 Sep 2020 |

Illustration
Scientists using a mathematical model to study the first months of the corona pandemic in Europe have found that the decrease of COVID-19 cases in spring was also related to the end of the flu season and influenza may have increased transmission of the coronavirus by an average of 2.5-fold.
The results of the study by scientists at the Max Planck Institute for Infection Biology (Berlin, Germany) and the Institut Pasteur (Paris, France) suggest that the coming flu epidemic will have an amplifying impact on the COVID-19 pandemic. The researchers have emphasized the potential importance of flu vaccinations as a possible extra protection against COVID-19.
Data from earlier experiments led the team to investigate the effects of a co-infection with coronavirus and flu. The researchers developed a mathematical model of coronavirus transmission and mortality to decipher the influence of the flu season on the COVID-19 pandemic. The researchers modelled the course of the pandemic in Belgium, Norway, Italy and Spain. Four European countries in which the pandemic was differently pronounced during the first half of the year. To approach the real infection events, the model was based on known disease parameters like the "generation interval", i.e. the time needed for an infected person to infect another person. The researchers also took non-pharmaceutical countermeasures into account, since lockdowns and social distancing had an extensive impact on the pandemic. This was measured by the so-called Stringency Index, a value developed by Oxford University, which indicates the "strictness" of government anti-coronavirus measures.
After mathematically recreating the pandemic, the researchers were able to test various assumptions about the impact of the flu season. They checked if the model was more realistic under the assumption that influenza either reduces, increases, or does not influence the transmission rate of coronavirus. The team showed that influenza may have increased coronavirus transmission at the population level by 2–2.5 times, on average during the period of co-circulation. The researchers checked their model against data on daily deaths in the four countries, enabling them to demonstrate that their model is consistent with the observed pandemic mortality data. Without the amplifying impact of influenza, the model explained the observed data substantially less well - with significantly lower COVID-19 infection rates.
It remains open whether influenza patients are more likely to transmit coronavirus to others or whether flu makes people more susceptible to corona, although the latter seems more probable according to the researchers. Other research groups recently showed that flu viruses may increase susceptibility to COVID-19 in patients: Influenza viruses cause a higher production of the receptors that are used by the coronavirus to dock to human respiratory cells. These results imply that vaccinating against influenza may be essential in the coming flu season, not only to relieve hospitals, but also to contain the potential effect of influenza on the transmission of coronavirus.
Related Links:
Max Planck Institute for Infection Biology
Institut Pasteur
The results of the study by scientists at the Max Planck Institute for Infection Biology (Berlin, Germany) and the Institut Pasteur (Paris, France) suggest that the coming flu epidemic will have an amplifying impact on the COVID-19 pandemic. The researchers have emphasized the potential importance of flu vaccinations as a possible extra protection against COVID-19.
Data from earlier experiments led the team to investigate the effects of a co-infection with coronavirus and flu. The researchers developed a mathematical model of coronavirus transmission and mortality to decipher the influence of the flu season on the COVID-19 pandemic. The researchers modelled the course of the pandemic in Belgium, Norway, Italy and Spain. Four European countries in which the pandemic was differently pronounced during the first half of the year. To approach the real infection events, the model was based on known disease parameters like the "generation interval", i.e. the time needed for an infected person to infect another person. The researchers also took non-pharmaceutical countermeasures into account, since lockdowns and social distancing had an extensive impact on the pandemic. This was measured by the so-called Stringency Index, a value developed by Oxford University, which indicates the "strictness" of government anti-coronavirus measures.
After mathematically recreating the pandemic, the researchers were able to test various assumptions about the impact of the flu season. They checked if the model was more realistic under the assumption that influenza either reduces, increases, or does not influence the transmission rate of coronavirus. The team showed that influenza may have increased coronavirus transmission at the population level by 2–2.5 times, on average during the period of co-circulation. The researchers checked their model against data on daily deaths in the four countries, enabling them to demonstrate that their model is consistent with the observed pandemic mortality data. Without the amplifying impact of influenza, the model explained the observed data substantially less well - with significantly lower COVID-19 infection rates.
It remains open whether influenza patients are more likely to transmit coronavirus to others or whether flu makes people more susceptible to corona, although the latter seems more probable according to the researchers. Other research groups recently showed that flu viruses may increase susceptibility to COVID-19 in patients: Influenza viruses cause a higher production of the receptors that are used by the coronavirus to dock to human respiratory cells. These results imply that vaccinating against influenza may be essential in the coming flu season, not only to relieve hospitals, but also to contain the potential effect of influenza on the transmission of coronavirus.
Related Links:
Max Planck Institute for Infection Biology
Institut Pasteur
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
Intestinal gases are associated with several health conditions, including colon cancer, irritable bowel syndrome, and inflammatory bowel disease, and they have the potential to serve as crucial biomarkers... Read moreNovel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
Multiphoton microscopy has become an invaluable tool in neuroscience, allowing researchers to observe brain activity in real time with high-resolution imaging. A crucial aspect of many multiphoton microscopy... Read more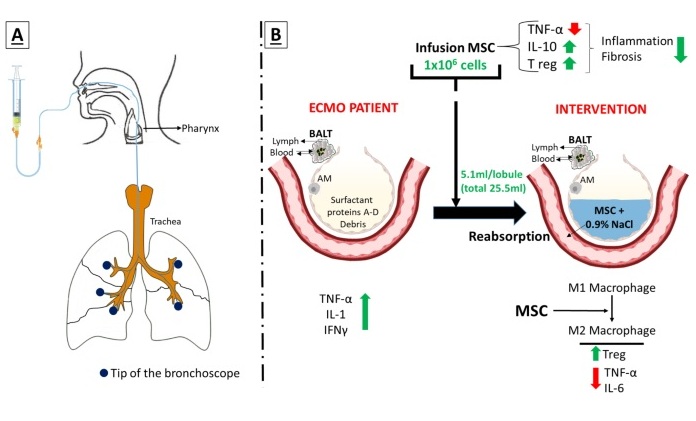
Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
Until now, administering cell therapies to patients on extracorporeal membrane oxygenation (ECMO)—a life-support system typically used for severe lung failure—has been nearly impossible.... Read moreSurgical Techniques
view channel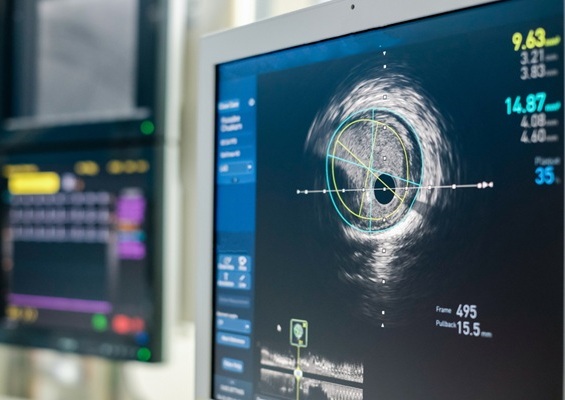
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more