New Artificial Intelligence Method Helps Design Better COVID-19 Antibody Drugs
|
By HospiMedica International staff writers Posted on 20 Apr 2021 |

Illustration
Machine learning methods can help to optimize the development of COVID-19 antibody drugs, leading to active substances with improved properties, also with regard to tolerability in the body, according to researchers.
Scientists at ETH Zürich (Zürich, Switzerland) have developed a machine learning method that supports the optimization phase, helping to develop more effective antibody drugs. Antibodies are not only produced by our immune cells to fight viruses and other pathogens in the body. For a few decades now, medicine has also been using antibodies produced by biotechnology as drugs. This is because antibodies are extremely good at binding specifically to molecular structures according to the lock-and-key principle. Their use ranges from oncology to the treatment of autoimmune diseases and neurodegenerative conditions.
However, developing such antibody drugs is anything but simple. The basic requirement is for an antibody to bind to its target molecule in an optimal way. At the same time, an antibody drug must fulfill a host of additional criteria. For example, it should not trigger an immune response in the body, it should be efficient to produce using biotechnology, and it should remain stable over a long period of time. Once scientists have found an antibody that binds to the desired molecular target structure, the development process is far from over. Rather, this marks the start of a phase in which researchers use bioengineering to try to improve the antibody’s properties.
When researchers optimize an entire antibody molecule in its therapeutic form (i.e. not just a fragment of an antibody), it used to start with an antibody lead candidate that binds reasonably well to the desired target structure. Then researchers randomly mutate the gene that carries the blueprint for the antibody in order to produce a few thousand related antibody candidates in the lab. The next step is to search among them to find the ones that bind best to the target structure. The ETH researchers are now using machine learning to increase the initial set of antibodies to be tested to several million.
The researchers provided the proof of concept for their new method using Roche’s antibody cancer drug Herceptin, which has been on the market for 20 years. Starting out from the DNA sequence of the Herceptin antibody, the ETH researchers created about 40,000 related antibodies using a CRISPR mutation method they developed a few years ago. Experiments showed that 10,000 of them bound well to the target protein in question, a specific cell surface protein. The scientists used the DNA sequences of these 40,000 antibodies to train a machine learning algorithm. They then applied the trained algorithm to search a database of 70 million potential antibody DNA sequences. For these 70 million candidates, the algorithm predicted how well the corresponding antibodies would bind to the target protein, resulting in a list of millions of sequences expected to bind.
Using further computer models, the scientists predicted how well these millions of sequences would meet the additional criteria for drug development (tolerance, production, physical properties). This reduced the number of candidate sequences to 8,000. From the list of optimized candidate sequences on their computer, the scientists selected 55 sequences from which to produce antibodies in the lab and characterize their properties. Subsequent experiments showed that several of them bound even better to the target protein than Herceptin itself, as well as being easier to produce and more stable than Herceptin. The ETH scientists are now applying their AI method to optimize antibody drugs that are in clinical development.
“With automated processes, you can test a few thousand therapeutic candidates in a lab. But it is not really feasible to screen any more than that,” said Sai Reddy, a professor at the Department of Biosystems Science and Engineering at ETH Zurich who led the study. “Typically, the best dozen antibodies from this screening move on to the next step and are tested for how well they meet additional criteria. “Ultimately, this approach lets you identify the best antibody from a group of a few thousand.”
Related Links:
ETH Zürich
Scientists at ETH Zürich (Zürich, Switzerland) have developed a machine learning method that supports the optimization phase, helping to develop more effective antibody drugs. Antibodies are not only produced by our immune cells to fight viruses and other pathogens in the body. For a few decades now, medicine has also been using antibodies produced by biotechnology as drugs. This is because antibodies are extremely good at binding specifically to molecular structures according to the lock-and-key principle. Their use ranges from oncology to the treatment of autoimmune diseases and neurodegenerative conditions.
However, developing such antibody drugs is anything but simple. The basic requirement is for an antibody to bind to its target molecule in an optimal way. At the same time, an antibody drug must fulfill a host of additional criteria. For example, it should not trigger an immune response in the body, it should be efficient to produce using biotechnology, and it should remain stable over a long period of time. Once scientists have found an antibody that binds to the desired molecular target structure, the development process is far from over. Rather, this marks the start of a phase in which researchers use bioengineering to try to improve the antibody’s properties.
When researchers optimize an entire antibody molecule in its therapeutic form (i.e. not just a fragment of an antibody), it used to start with an antibody lead candidate that binds reasonably well to the desired target structure. Then researchers randomly mutate the gene that carries the blueprint for the antibody in order to produce a few thousand related antibody candidates in the lab. The next step is to search among them to find the ones that bind best to the target structure. The ETH researchers are now using machine learning to increase the initial set of antibodies to be tested to several million.
The researchers provided the proof of concept for their new method using Roche’s antibody cancer drug Herceptin, which has been on the market for 20 years. Starting out from the DNA sequence of the Herceptin antibody, the ETH researchers created about 40,000 related antibodies using a CRISPR mutation method they developed a few years ago. Experiments showed that 10,000 of them bound well to the target protein in question, a specific cell surface protein. The scientists used the DNA sequences of these 40,000 antibodies to train a machine learning algorithm. They then applied the trained algorithm to search a database of 70 million potential antibody DNA sequences. For these 70 million candidates, the algorithm predicted how well the corresponding antibodies would bind to the target protein, resulting in a list of millions of sequences expected to bind.
Using further computer models, the scientists predicted how well these millions of sequences would meet the additional criteria for drug development (tolerance, production, physical properties). This reduced the number of candidate sequences to 8,000. From the list of optimized candidate sequences on their computer, the scientists selected 55 sequences from which to produce antibodies in the lab and characterize their properties. Subsequent experiments showed that several of them bound even better to the target protein than Herceptin itself, as well as being easier to produce and more stable than Herceptin. The ETH scientists are now applying their AI method to optimize antibody drugs that are in clinical development.
“With automated processes, you can test a few thousand therapeutic candidates in a lab. But it is not really feasible to screen any more than that,” said Sai Reddy, a professor at the Department of Biosystems Science and Engineering at ETH Zurich who led the study. “Typically, the best dozen antibodies from this screening move on to the next step and are tested for how well they meet additional criteria. “Ultimately, this approach lets you identify the best antibody from a group of a few thousand.”
Related Links:
ETH Zürich
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
Ingestible Capsule Monitors Intestinal Inflammation
Acute mesenteric ischemia—a life-threatening condition caused by blocked blood flow to the intestines—remains difficult to diagnose early because its symptoms often mimic common digestive problems.... Read more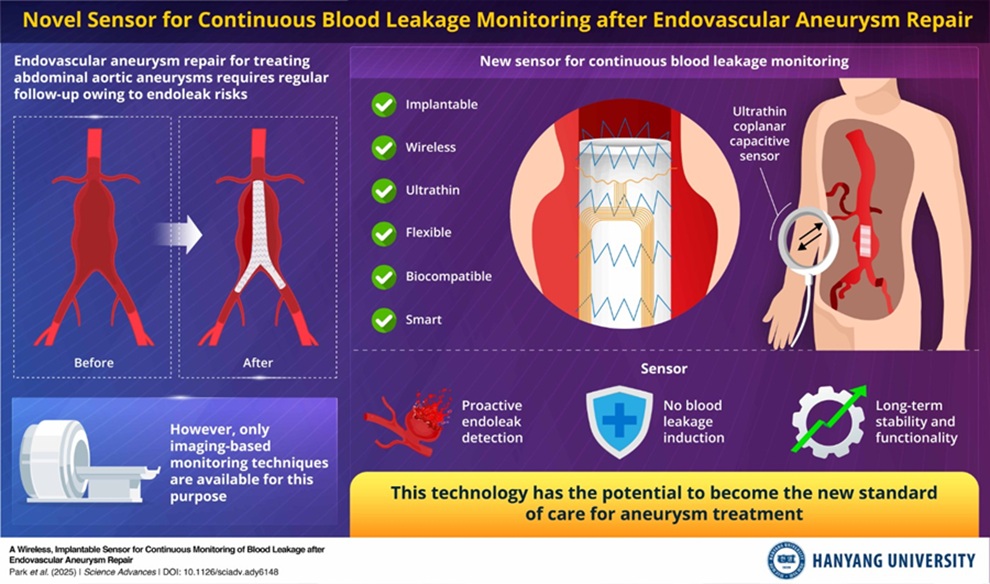
Wireless Implantable Sensor Enables Continuous Endoleak Monitoring
Endovascular aneurysm repair (EVAR) is a life-saving, minimally invasive treatment for abdominal aortic aneurysms—balloon-like bulges in the aorta that can rupture with fatal consequences.... Read more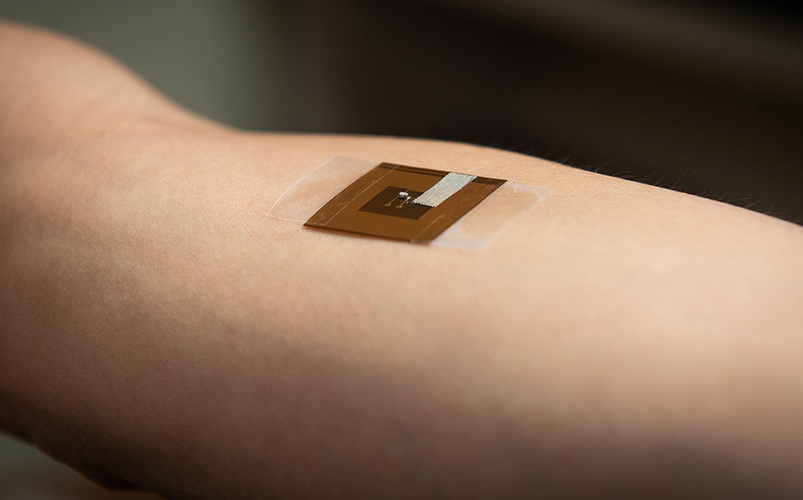
Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
Skin cancer remains one of the most dangerous and common cancers worldwide, with early detection crucial for improving survival rates. Traditional diagnostic methods—visual inspections, imaging, and biopsies—can... Read moreSurgical Techniques
view channel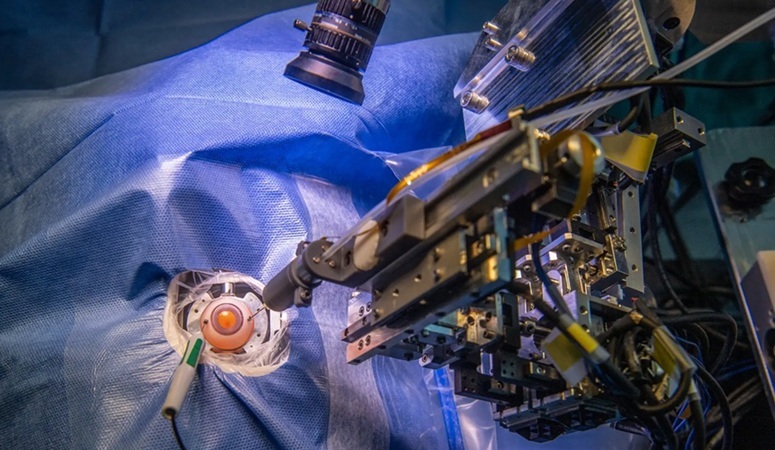
Robotic Assistant Delivers Ultra-Precision Injections with Rapid Setup Times
Age-related macular degeneration (AMD) is a leading cause of blindness worldwide, affecting nearly 200 million people, a figure expected to rise to 280 million by 2040. Current treatment involves doctors... Read more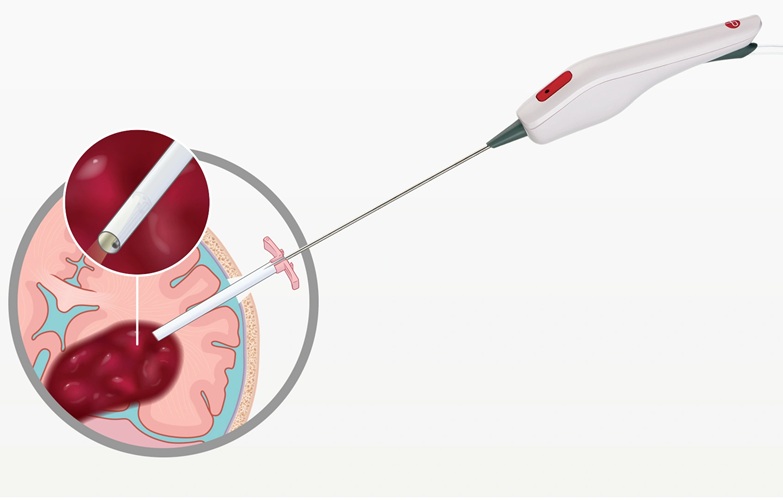
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more
















