ECMO Life Support Offers Sickest COVID-19 Patients Slimmer Chance of Survival than Once Thought
|
By HospiMedica International staff writers Posted on 01 Oct 2021 |

The life-support system called ECMO (extracorporeal membrane oxygenation) can rescue COVID-19 patients from the brink of death, but not at the rates seen early in the pandemic, a new international study has found.
The new findings of the study by researchers at the University of Michigan (Ann Arbor, MI, USA) used data from more than 4,800 patients over age 16 who were treated with ECMO for advanced COVID-19 in 41 countries during 2020. The study found that where once about 60% of such patients survived at least 90 days in spring 2020, by the end of the year just under half of COVID patients on ECMO survived that long. The decreased survival over time might be due to a combination of factors, including which critically ill patients clinicians chose to place on ECMO as the pandemic went on, and the treatments the patients had received before they started on ECMO. The new findings show how important it is for hospitals that offer ECMO to choose carefully which patients get access to this labor-intensive level of care. Hospitals should also make policies that can guide such choices when ECMO circuits are in high demand because of a pandemic surge, according to the researchers.
ECMO has been used for decades in select hospitals to treat critically ill children and adults. It takes over for both the heart and lungs temporarily, circulating the blood outside the body under constant supervision of trained providers. At the start of the pandemic, some experts had strong reservations about placing COVID-19 patients on ECMO, for fear of harming their lungs. As more centers began to try it, the survival rate mirrored that of ECMO’s use in other forms of acute lung failure, as the team behind the new study had reported a year ago.
The new study divided the patients into three groups: those treated before May 1, 2020, those treated in these “early adopter” hospitals after May 1, and those treated with ECMO in other hospitals from May 1 through the end of 2020. May 1 was chosen because the evidence for how best to treat critically ill COVID-19 patients had evolved considerably by then. Within the “early adopter” centers, mortality rates increased from 37% in the months before May, to 52% after May. At the centers that did not start providing ECMO until at least May, 58% of the patients died within 90 days of being placed on an ECMO circuit. Patients treated with ECMO later in the pandemic were more likely to have received medications such as remdesivir and dexamethasone, and to have received non-invasive ventilation before being intubated for total breathing support.
Having patients stay on ECMO for a longer time ties up many resources, including the machines and tubing that make up an ECMO circuit, and the specially trained nurses, respiratory therapists and other staff it takes to keep a circuit operating safely. When a hospital has a large number of COVID-19 patients and others in intensive care, the team’s ability to provide the same level of care that they did before the surge can suffer, and mortality might increase. If many hospitals in a region or collection of states are coping with a large number of critically ill COVID-19 patients, it can be hard to find an ECMO-capable hospital to transfer patients to. Sending more ECMO circuits - the pumps, tubes and controllers used in the treatment - to these hospitals is not sufficient; specially trained teams, adequate blood supply and other factors are all needed to support each ECMO patient. This makes it important for ECMO centers to carefully consider which risk factors and personal characteristics might make a patient more or less likely to survive if placed on ECMO, especially if they might need to be on for a while.
“What we noticed right away is that the patients treated later in the pandemic were staying on ECMO longer, going from an average of 14 days to 20 days. They were dying more often, and these deaths were different,” said Ryan Barbaro, M.D., M.S., associate professor at the U-M Medical School and intensive care physician at Michigan Medicine, the University of Michigan’s academic medical center. “This shows that we need to be thoughtful about who we’re putting on ECMO and when we’re making the decision to take patients off who aren’t getting better. Across the U.S. right now, we have places where ECMO is a scarce resource whereas in Michigan it’s not quite at that point, but we anticipate it might be.”
Related Links:
University of Michigan
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel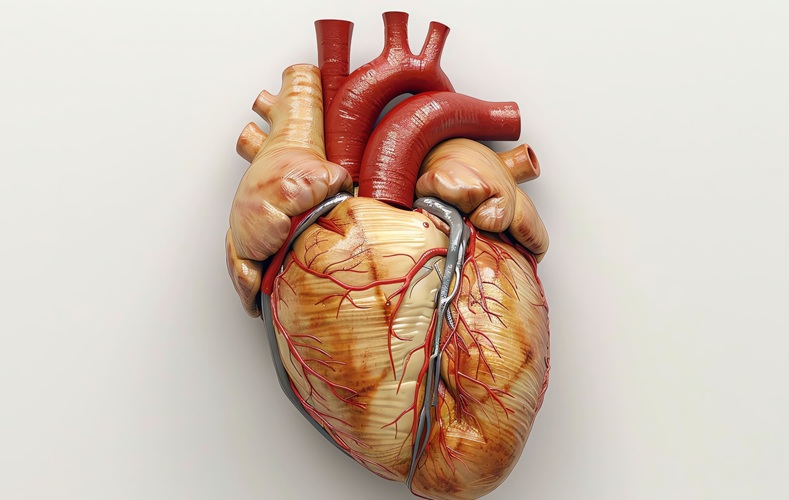
Mechanosensing-Based Approach Offers Promising Strategy to Treat Cardiovascular Fibrosis
Cardiac fibrosis, which involves the stiffening and scarring of heart tissue, is a fundamental feature of nearly every type of heart disease, from acute ischemic injuries to genetic cardiomyopathies.... Read more
AI Interpretability Tool for Photographed ECG Images Offers Pixel-Level Precision
The electrocardiogram (ECG) is a crucial diagnostic tool in modern medicine, used to detect heart conditions such as arrhythmias and structural abnormalities. Every year, millions of ECGs are performed... Read moreSurgical Techniques
view channel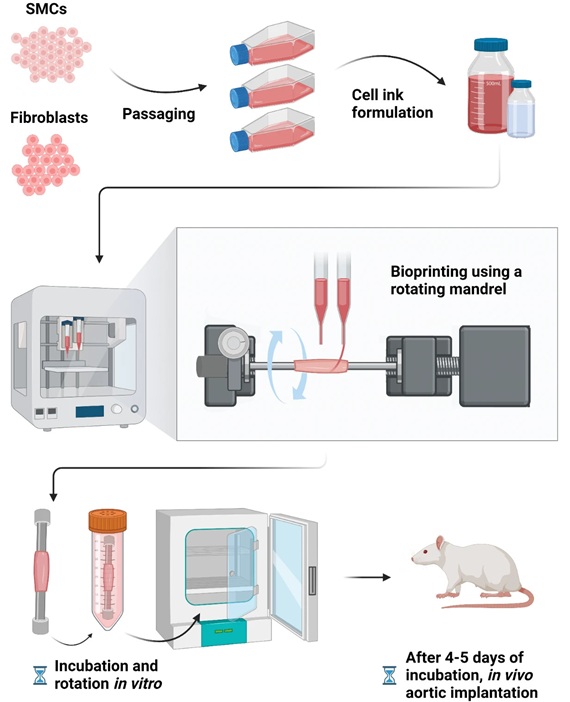
Bioprinted Aortas Offer New Hope for Vascular Repair
Current treatment options for severe cardiovascular diseases include using grafts made from a patient's own tissue (autologous) or synthetic materials. However, autologous grafts require invasive surgery... Read more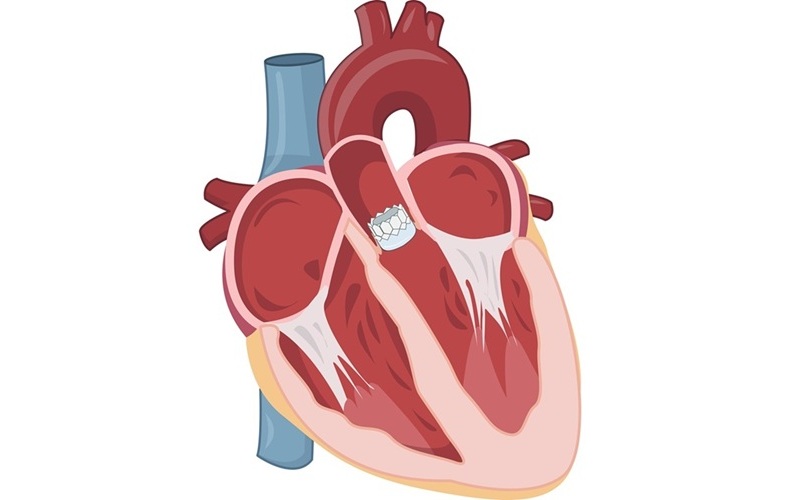
Early TAVR Intervention Reduces Cardiovascular Events in Asymptomatic Aortic Stenosis Patients
Each year, approximately 300,000 Americans are diagnosed with aortic stenosis (AS), a serious condition that results from the narrowing or blockage of the aortic valve in the heart. Two common treatments... Read more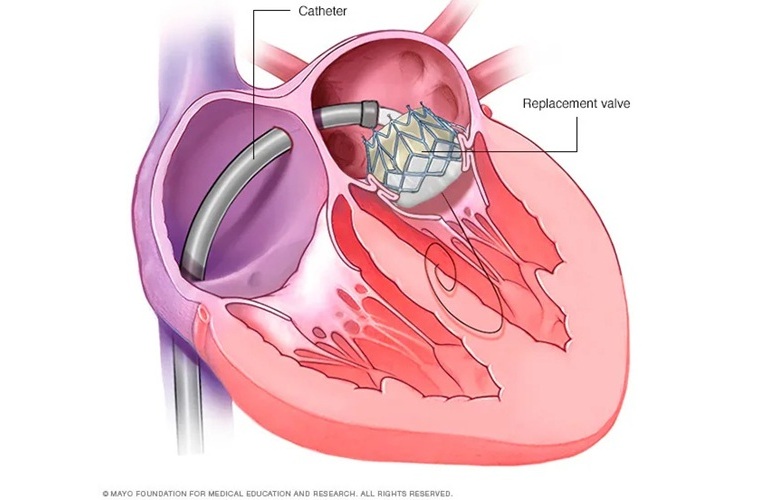
New Procedure Found Safe and Effective for Patients Undergoing Transcatheter Mitral Valve Replacement
In the United States, approximately four million people suffer from mitral valve regurgitation, the most common type of heart valve disease. As an alternative to open-heart surgery, transcatheter mitral... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more



















