Testing for SARS-CoV-2 Blood Antigen Levels Can Predict Clinical Outcomes of COVID-19 Patients
|
By HospiMedica International staff writers Posted on 02 Sep 2022 |
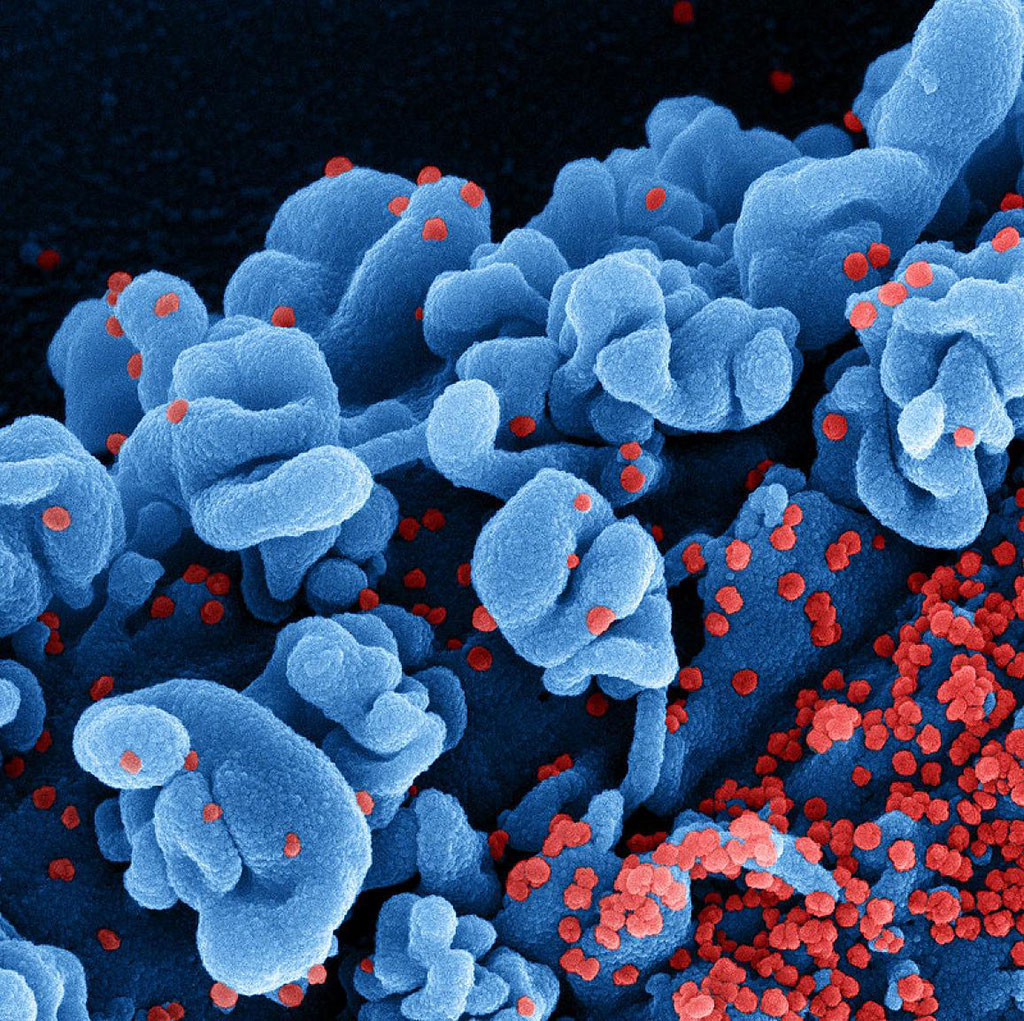
The amount of SARS-CoV-2 antigen measured in the blood of patients hospitalized with COVID-19 is associated with illness severity and other clinical outcomes, according to a new study. Following the ACTIV-3 trial of COVID-19 therapeutics in people hospitalized with COVID-19, researchers from the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH, Bethesda, MD, USA), and their collaborators analyzed levels of SARS-COV-2 antigen in blood samples taken from study participants and assessed the association of those levels with disease progression. Higher levels of viral antigen in the blood, which could indicate ongoing SARS-CoV-2 replication, correlated with more severe disease. The researchers suggest that SARS-CoV-2 antigen levels hold promise as a biomarker, or a measurable substance, to predict which patients hospitalized with COVID-19 have a higher risk of worse outcomes.
The ACTIV-3 trial enrolled people hospitalized with COVID-19 between August 2020 and November 2021. Participants contributed a baseline blood sample and were then randomized to receive either an experimental COVID-19 therapeutic or a placebo. All participants received the antiviral remdesivir unless contraindicated. In this follow-up analysis, the researchers examined 2,540 participant baseline blood samples for SARS-CoV-2 antigen levels. The researchers assessed the relationship between each participant’s SARS-CoV-2 blood antigen levels and their time to discharge from the hospital, as well as their pulmonary symptoms at day five of the trial - whether they had stayed the same, worsened, or improved since enrollment.
With all this information in hand, the researchers conducted statistical analyses to determine if plasma antigen levels were associated with the participants’ pulmonary function when they gave the blood sample - and whether they could predict how the participants would fare over time. In addition, the researchers examined the relationship between a number of participant and viral characteristics and antigen levels. The analysis revealed a strong correlation between higher SARS-CoV-2 antigen levels (≥1000 nanograms per liter) and worse pulmonary function at the time of enrollment. Importantly, participants with higher SARS-CoV-2 antigen levels in the blood at enrollment generally had decreased pulmonary function at day five, regardless of the severity of their illness at the time of study entry, and took longer to be released from the hospital.
High blood antigen levels also correlated with some known risk factors for worse illness, such as being male. Three additional participant characteristics were found to correlate with lower antigen levels: the presence of SARS-CoV-2 antibodies, exposure to remdesivir prior to enrollment and longer time in hospital prior to enrollment. Finally, participants infected with the delta variant had higher antigen levels than those infected with prior circulating strains. The researchers concluded that antigen levels in the blood are likely a marker of ongoing viral replication and could be useful for predicting a patient’s disease progression and likely outcomes once they are admitted to the hospital. The researchers note that these results suggest that a precision medicine approach could be helpful in future clinical trials of antiviral therapy. For instance, antigen levels could help determine those patients most likely to benefit from therapies directed at fighting the virus.
Related Links:
National Institutes of Health
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read more
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read moreSurgical Techniques
view channel
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read more
Novel Glue Prevents Complications After Breast Cancer Surgery
Seroma and prolonged lymphorrhea are among the most common complications following axillary lymphadenectomy in breast cancer patients. These postoperative issues can delay recovery and postpone the start... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more