Automated System Identifies Ventilated Patients at Risk
|
By HospiMedica International staff writers Posted on 12 Jun 2018 |
An automated system for detecting mechanically ventilated patients at risk of ventilator-associated events surpasses traditional surveillance methods, according to a new study.
Developed at Massachusetts General Hospital (MGH; Boston, USA), the Georgia Institute of Technology (Atlanta, USA), and Harvard Medical School (HMS; Boston, MA, USA), the automated process uses an algorithm that analyses physiologic data to detect increases in positive end-expiratory pressure (PEEP) and fraction of inspired oxygen (FiO2); queries the electronic health record (EHR) for leukopenia or leukocytosis and antibiotic initiation data; and retrieves and interprets microbiology reports.
Based on the data, the algorithm can determine whether criteria were met for a ventilator-associated event and, if so, which level of event:
• A ventilator-associated condition (VAC), an increase in a patient's need for oxygen without evidence of infection.
• An infection-related ventilator-associated complication (IVAC), with increased oxygen need accompanied by signs of infection, such as fever, elevated white blood cell count or an antibiotic prescription.
• And possible ventilator-associated pneumonia (VAP), with evidence of bacterial growth in the respiratory system, along with the factors listed above.
A validation study to test the algorithm followed 1,234 patients admitted to the intensive care unit (ICU), 431 of who received ventilator support. During that period, manual surveillance produced accuracies of 71%, 98% and 87%, respectively, while results for the automated system were 85%, 99% and 100% accuracy. The drop-off in accuracy of the automated system during the validation period was the result a temporary interruption of data availability while software was being upgraded. The study was published on May 17, 2018, in Infection Control & Hospital Epidemiology.
“Manual surveillance made many more errors than automated surveillance, including false positives, reporting cases that on review, did not meet criteria for what are called ventilator-associated events; misclassifications, reporting an event as more or less serious than it really was; and failure to detect and report cases that, on closer inspection, actually met criteria,” said lead author Erica Shenoy, MD, PhD, of the MGH division of infectious diseases. “In contrast, so long as the necessary electronic data were available, the automated method performed perfectly.”
Traditional surveillance of patients receiving mechanical ventilation involves manual recording of ventilator settings every 12 hours and adjusted throughout the day to accommodate the patient's needs. The settings, which reflect the pressure required to keep a patient's lungs open at the end of a breath and the percentage of oxygen being delivered to the patient, are reviewed by an infection control practitioner for signs that indicate possible VAP.
Related Links:
Massachusetts General Hospital
Georgia Institute of Technology
Harvard Medical School
Developed at Massachusetts General Hospital (MGH; Boston, USA), the Georgia Institute of Technology (Atlanta, USA), and Harvard Medical School (HMS; Boston, MA, USA), the automated process uses an algorithm that analyses physiologic data to detect increases in positive end-expiratory pressure (PEEP) and fraction of inspired oxygen (FiO2); queries the electronic health record (EHR) for leukopenia or leukocytosis and antibiotic initiation data; and retrieves and interprets microbiology reports.
Based on the data, the algorithm can determine whether criteria were met for a ventilator-associated event and, if so, which level of event:
• A ventilator-associated condition (VAC), an increase in a patient's need for oxygen without evidence of infection.
• An infection-related ventilator-associated complication (IVAC), with increased oxygen need accompanied by signs of infection, such as fever, elevated white blood cell count or an antibiotic prescription.
• And possible ventilator-associated pneumonia (VAP), with evidence of bacterial growth in the respiratory system, along with the factors listed above.
A validation study to test the algorithm followed 1,234 patients admitted to the intensive care unit (ICU), 431 of who received ventilator support. During that period, manual surveillance produced accuracies of 71%, 98% and 87%, respectively, while results for the automated system were 85%, 99% and 100% accuracy. The drop-off in accuracy of the automated system during the validation period was the result a temporary interruption of data availability while software was being upgraded. The study was published on May 17, 2018, in Infection Control & Hospital Epidemiology.
“Manual surveillance made many more errors than automated surveillance, including false positives, reporting cases that on review, did not meet criteria for what are called ventilator-associated events; misclassifications, reporting an event as more or less serious than it really was; and failure to detect and report cases that, on closer inspection, actually met criteria,” said lead author Erica Shenoy, MD, PhD, of the MGH division of infectious diseases. “In contrast, so long as the necessary electronic data were available, the automated method performed perfectly.”
Traditional surveillance of patients receiving mechanical ventilation involves manual recording of ventilator settings every 12 hours and adjusted throughout the day to accommodate the patient's needs. The settings, which reflect the pressure required to keep a patient's lungs open at the end of a breath and the percentage of oxygen being delivered to the patient, are reviewed by an infection control practitioner for signs that indicate possible VAP.
Related Links:
Massachusetts General Hospital
Georgia Institute of Technology
Harvard Medical School
Latest Critical Care News
- One-Hour Endoscopic Procedure Could Eliminate Need for Insulin for Type 2 Diabetes
- AI Can Prioritize Emergecny Department Patients Requiring Urgent Treatment
- AI to Improve Diagnosis of Atrial Fibrillation
- Stretchable Microneedles to Help In Accurate Tracking of Abnormalities and Identifying Rapid Treatment
- Machine Learning Tool Identifies Rare, Undiagnosed Immune Disorders from Patient EHRs
- On-Skin Wearable Bioelectronic Device Paves Way for Intelligent Implants
- First-Of-Its-Kind Dissolvable Stent to Improve Outcomes for Patients with Severe PAD
- AI Brain-Age Estimation Technology Uses EEG Scans to Screen for Degenerative Diseases
- Wheeze-Counting Wearable Device Monitors Patient's Breathing In Real Time
- Wearable Multiplex Biosensors Could Revolutionize COPD Management
- New Low-Energy Defibrillation Method Controls Cardiac Arrhythmias
- New Machine Learning Models Help Predict Heart Disease Risk in Women
- Deep-Learning Model Predicts Arrhythmia 30 Minutes before Onset
- Breakthrough Technology Combines Detection and Treatment of Nerve-Related Disorders in Single Procedure
- Plasma Irradiation Promotes Faster Bone Healing
- New Device Treats Acute Kidney Injury from Sepsis
Channels
Artificial Intelligence
view channel
AI-Powered Algorithm to Revolutionize Detection of Atrial Fibrillation
Atrial fibrillation (AFib), a condition characterized by an irregular and often rapid heart rate, is linked to increased risks of stroke and heart failure. This is because the irregular heartbeat in AFib... Read more
AI Diagnostic Tool Accurately Detects Valvular Disorders Often Missed by Doctors
Doctors generally use stethoscopes to listen for the characteristic lub-dub sounds made by heart valves opening and closing. They also listen for less prominent sounds that indicate problems with these valves.... Read moreSurgical Techniques
view channel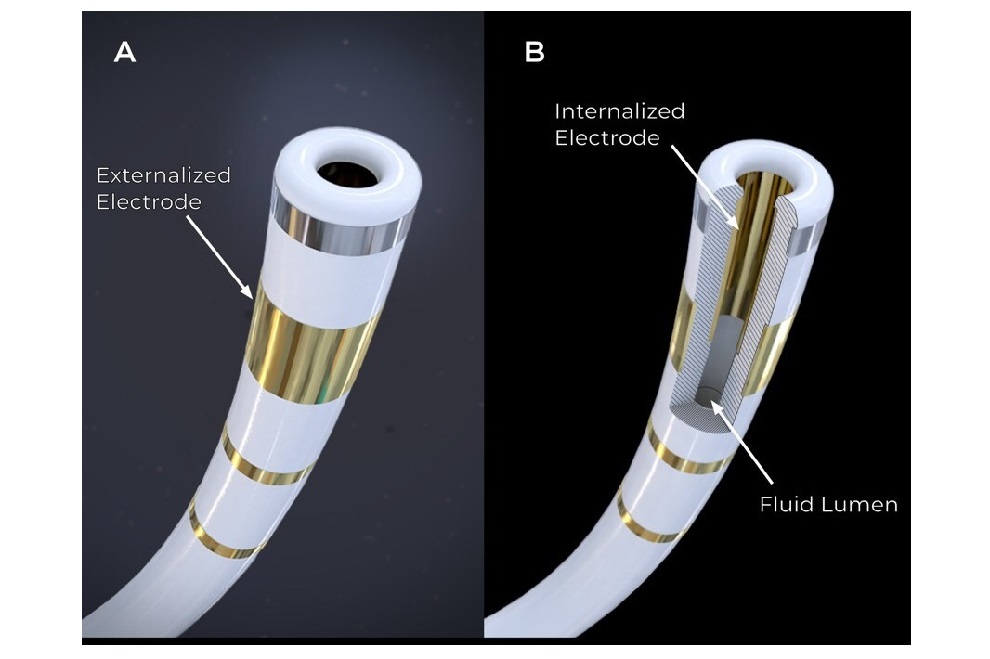
First-Ever Contact Force Pulsed Field Ablation System to Transform Treatment of Ventricular Arrhythmias
It is estimated that over 6 million patients in the US and Europe are affected by ventricular arrhythmias, which include conditions such as ventricular tachycardia (VT) and premature ventricular contractions (PVCs).... Read more
Caterpillar Robot with Built-In Steering System Crawls Easily Through Loops and Bends
Soft robots often face challenges in being guided effectively because adding steering mechanisms typically reduces their flexibility by increasing rigidity. Now, a team of engineers has combined ancient... Read more
Tiny Wraparound Electronic Implants to Revolutionize Treatment of Spinal Cord Injuries
The spinal cord functions as a vital conduit, transmitting nerve impulses to and from the brain, much like a highway. When the spinal cord is damaged, this flow of information is disrupted, leading to... Read morePatient Care
view channelFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more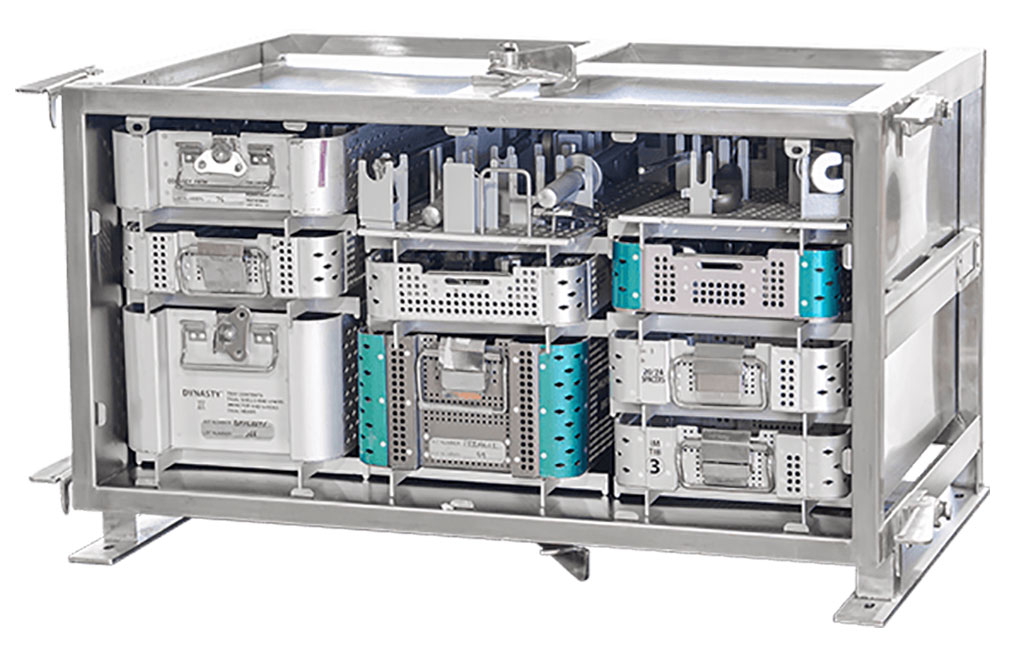
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel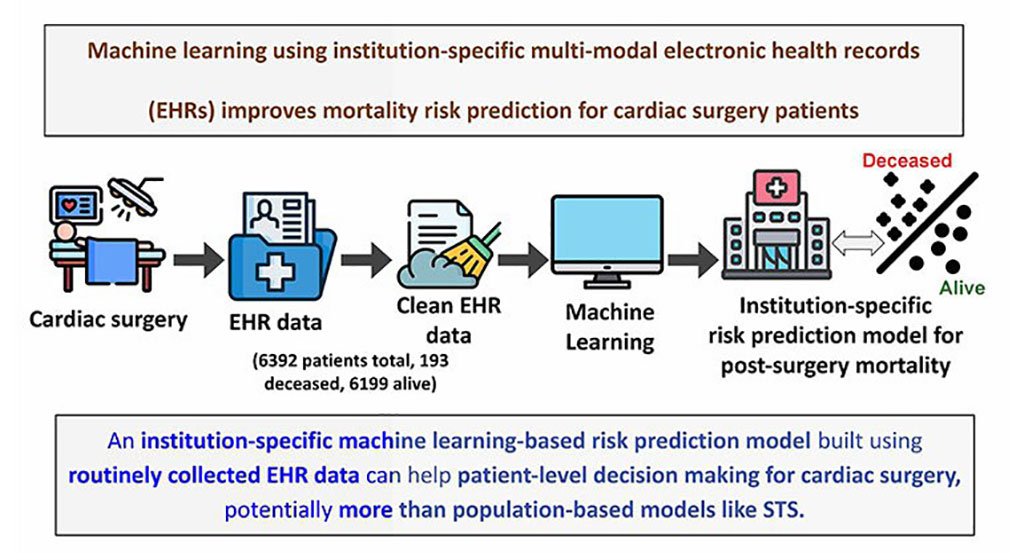
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read more
Point of Care HIV Test Enables Early Infection Diagnosis for Infants
Early diagnosis and initiation of treatment are crucial for the survival of infants infected with HIV (human immunodeficiency virus). Without treatment, approximately 50% of infants who acquire HIV during... Read more
Whole Blood Rapid Test Aids Assessment of Concussion at Patient's Bedside
In the United States annually, approximately five million individuals seek emergency department care for traumatic brain injuries (TBIs), yet over half of those suspecting a concussion may never get it checked.... Read more
New Generation Glucose Hospital Meter System Ensures Accurate, Interference-Free and Safe Use
A new generation glucose hospital meter system now comes with several features that make hospital glucose testing easier and more secure while continuing to offer accuracy, freedom from interference, and... Read moreBusiness
view channel
Johnson & Johnson Acquires Cardiovascular Medical Device Company Shockwave Medical
Johnson & Johnson (New Brunswick, N.J., USA) and Shockwave Medical (Santa Clara, CA, USA) have entered into a definitive agreement under which Johnson & Johnson will acquire all of Shockwave’s... Read more