Micro-Engineered Membrane Reduces Pacemaker Tissue Fibrosis
|
By HospiMedica International staff writers Posted on 02 Dec 2019 |

Image: A cellulose membrane can protecting pacemakers (Photo courtesy of Hylomorph/ ETH)
A protective membrane made of biosynthesized cellulose (BC) significantly reduces the build-up of fibrotic tissue around implanted cardiac pacemakers, according to a new study.
Developed at the Swiss Federal Institute of Technology (ETH; Zurich, Switzerland), the German Centre for Cardiovascular Research (DZHK; Berlin, Germany), Charité University Medicine (Charité; Berlin, Germany), and other institutions, the micro-engineered non-resorbable BC membrane was created by transferring surface microscale geometries via a lithographic protocol harnessing the fermentation process. Symmetric arrays of hexagonal pits in the micron range were generated onto the BC surface in order to interfere with the adhesion of cells involved in foreign body reaction, including fibroblasts and macrophages.
The researchers tested the membrane on 16 pigs; two pacemakers were implanted in each, of which one was enveloped in the cellulose membrane; the pacemakers were explanted at three and 12 months. Analysis showed that the BC protective layers were undamaged, with no sign of chemical or mechanical degradation. They appeared as a thin white-tan layer adherent to the surrounding thin fibrous capsule, from which it could be peeled off by gently pulling with forceps. An average reduction of 66% in fibrotic tissue thickness around the pacemaker was shown, and both the generator and the proximal parts of the leads were completely free of fibrotic tissue. The study was published on October 31, 2109, in Biomaterials.
“When fibrotic tissue forms, the first stage is the deposition of proteins on the surface; a fibrous membrane surface impedes this process. Another factor is that the membrane has honeycomb-like indentations in the surface, each measuring 10 micrometres in diameter,” said lead author Francesco Robotti, PhD, of ETH. “These indentations make it difficult for the cells that form fibrotic tissue to adhere to the surface, creating the conditions for simplified implantable electronic device revision surgeries.”
“Every pacemaker has to be replaced at some point. When this time comes, typically after about five years when the device's battery expires, the patient has to undergo surgery,” said co-senior author Aldo Ferrari, PhD, of ETH and Empa. “If too much fibrotic tissue has formed around the pacemaker, it complicates the procedure. In such cases, the surgeon has to cut into and remove this excess tissue. Not only does that prolong the operation, it also increases the risk of complications such as infection.”
Upon cardiac implantable electronic device (CIED) exchange, upgrade, or revision surgery, patients are exposed to a considerable risk of adverse events. The presence of firm fibrotic tissue endangers these procedures. Leads can be damaged in the attempt of freeing them from fibrotic tissue, and hematoma can form as result of capsulectomy, pocket debridement, and leads dissection. Due to the increasing number of CIED exchange, upgrade, and revision surgeries, the incidence of related complications is expected to rise in the near future.
Related Links:
Swiss Federal Institute of Technology
German Centre for Cardiovascular Research
Charité University Medicine
Developed at the Swiss Federal Institute of Technology (ETH; Zurich, Switzerland), the German Centre for Cardiovascular Research (DZHK; Berlin, Germany), Charité University Medicine (Charité; Berlin, Germany), and other institutions, the micro-engineered non-resorbable BC membrane was created by transferring surface microscale geometries via a lithographic protocol harnessing the fermentation process. Symmetric arrays of hexagonal pits in the micron range were generated onto the BC surface in order to interfere with the adhesion of cells involved in foreign body reaction, including fibroblasts and macrophages.
The researchers tested the membrane on 16 pigs; two pacemakers were implanted in each, of which one was enveloped in the cellulose membrane; the pacemakers were explanted at three and 12 months. Analysis showed that the BC protective layers were undamaged, with no sign of chemical or mechanical degradation. They appeared as a thin white-tan layer adherent to the surrounding thin fibrous capsule, from which it could be peeled off by gently pulling with forceps. An average reduction of 66% in fibrotic tissue thickness around the pacemaker was shown, and both the generator and the proximal parts of the leads were completely free of fibrotic tissue. The study was published on October 31, 2109, in Biomaterials.
“When fibrotic tissue forms, the first stage is the deposition of proteins on the surface; a fibrous membrane surface impedes this process. Another factor is that the membrane has honeycomb-like indentations in the surface, each measuring 10 micrometres in diameter,” said lead author Francesco Robotti, PhD, of ETH. “These indentations make it difficult for the cells that form fibrotic tissue to adhere to the surface, creating the conditions for simplified implantable electronic device revision surgeries.”
“Every pacemaker has to be replaced at some point. When this time comes, typically after about five years when the device's battery expires, the patient has to undergo surgery,” said co-senior author Aldo Ferrari, PhD, of ETH and Empa. “If too much fibrotic tissue has formed around the pacemaker, it complicates the procedure. In such cases, the surgeon has to cut into and remove this excess tissue. Not only does that prolong the operation, it also increases the risk of complications such as infection.”
Upon cardiac implantable electronic device (CIED) exchange, upgrade, or revision surgery, patients are exposed to a considerable risk of adverse events. The presence of firm fibrotic tissue endangers these procedures. Leads can be damaged in the attempt of freeing them from fibrotic tissue, and hematoma can form as result of capsulectomy, pocket debridement, and leads dissection. Due to the increasing number of CIED exchange, upgrade, and revision surgeries, the incidence of related complications is expected to rise in the near future.
Related Links:
Swiss Federal Institute of Technology
German Centre for Cardiovascular Research
Charité University Medicine
Latest Surgical Techniques News
- Porous Gel Sponge Facilitates Rapid Hemostasis and Wound Healing
- Novel Rigid Endoscope System Enables Deep Tissue Imaging During Surgery
- Robotic Nerve ‘Cuffs’ Could Treat Various Neurological Conditions
- Flexible Microdisplay Visualizes Brain Activity in Real-Time To Guide Neurosurgeons

- Next-Gen Computer Assisted Vacuum Thrombectomy Technology Rapidly Removes Blood Clots
- Hydrogel-Based Miniaturized Electric Generators to Power Biomedical Devices
- Custom 3D-Printed Orthopedic Implants Transform Joint Replacement Surgery
- Wearable Technology Monitors and Analyzes Surgeons' Posture during Long Surgical Procedures
- Cutting-Edge Imaging Platform Detects Residual Breast Cancer Missed During Lumpectomy Surgery
- Computational Models Predict Heart Valve Leakage in Children
- Breakthrough Device Enables Clear and Real-Time Visual Guidance for Effective Cardiovascular Interventions
- World’s First Microscopic Probe to Revolutionize Early Cancer Diagnosis
- World’s Smallest Implantable Brain Stimulator Demonstrated in Human Patient

- Robotically Assisted Lung Transplants Could Soon Become a Reality
- AI to Provide Heart Transplant Surgeons with New Decision-Making Data
- New Surgical Tool Empowers Precision and Confidence in Operating Room
Channels
Artificial Intelligence
view channel
AI-Powered Algorithm to Revolutionize Detection of Atrial Fibrillation
Atrial fibrillation (AFib), a condition characterized by an irregular and often rapid heart rate, is linked to increased risks of stroke and heart failure. This is because the irregular heartbeat in AFib... Read more
AI Diagnostic Tool Accurately Detects Valvular Disorders Often Missed by Doctors
Doctors generally use stethoscopes to listen for the characteristic lub-dub sounds made by heart valves opening and closing. They also listen for less prominent sounds that indicate problems with these valves.... Read moreCritical Care
view channel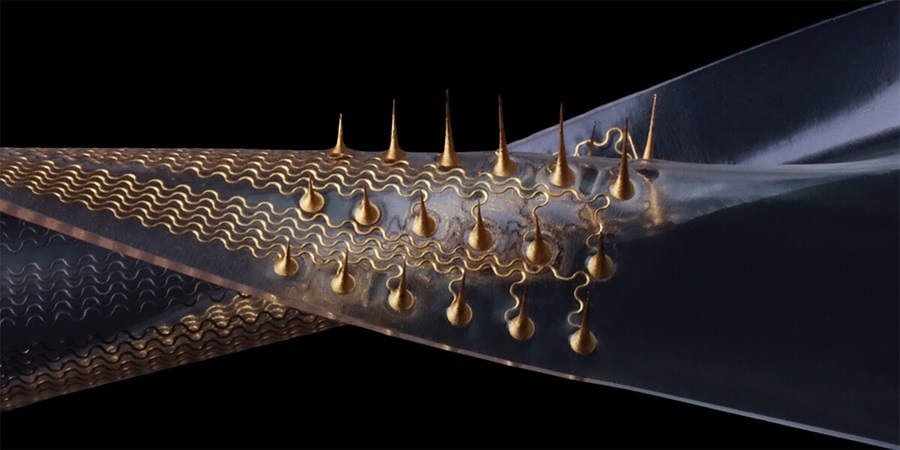
Stretchable Microneedles to Help In Accurate Tracking of Abnormalities and Identifying Rapid Treatment
The field of personalized medicine is transforming rapidly, with advancements like wearable devices and home testing kits making it increasingly easy to monitor a wide range of health metrics, from heart... Read more
Machine Learning Tool Identifies Rare, Undiagnosed Immune Disorders from Patient EHRs
Patients suffering from rare diseases often endure extensive delays in receiving accurate diagnoses and treatments, which can lead to unnecessary tests, worsening health, psychological strain, and significant... Read more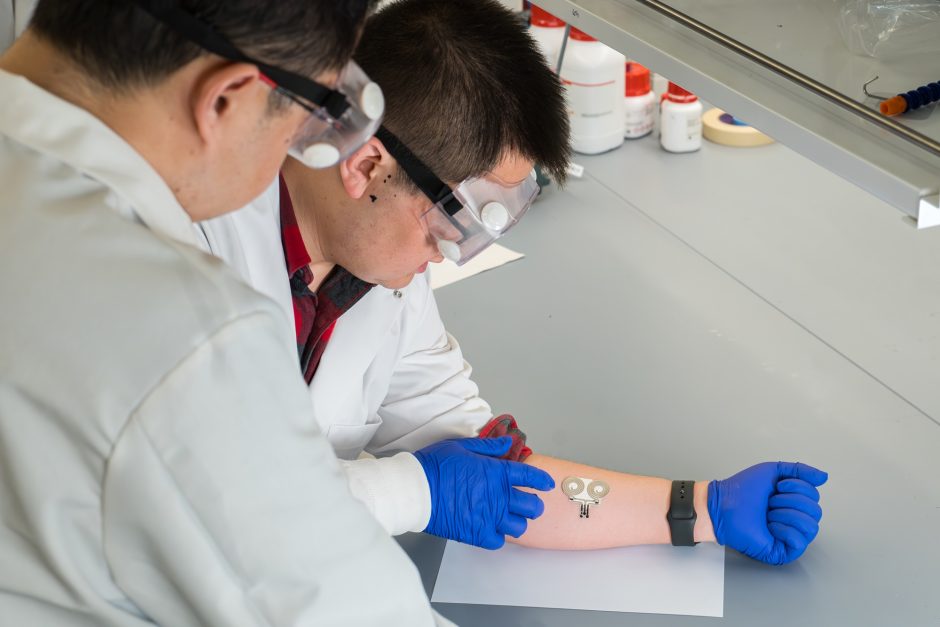
On-Skin Wearable Bioelectronic Device Paves Way for Intelligent Implants
A team of researchers at the University of Missouri (Columbia, MO, USA) has achieved a milestone in developing a state-of-the-art on-skin wearable bioelectronic device. This development comes from a lab... Read more
First-Of-Its-Kind Dissolvable Stent to Improve Outcomes for Patients with Severe PAD
Peripheral artery disease (PAD) affects millions and presents serious health risks, particularly its severe form, chronic limb-threatening ischemia (CLTI). CLTI develops when arteries are blocked by plaque,... Read morePatient Care
view channelFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read more
Point of Care HIV Test Enables Early Infection Diagnosis for Infants
Early diagnosis and initiation of treatment are crucial for the survival of infants infected with HIV (human immunodeficiency virus). Without treatment, approximately 50% of infants who acquire HIV during... Read more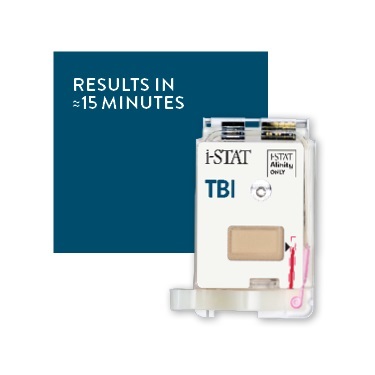
Whole Blood Rapid Test Aids Assessment of Concussion at Patient's Bedside
In the United States annually, approximately five million individuals seek emergency department care for traumatic brain injuries (TBIs), yet over half of those suspecting a concussion may never get it checked.... Read more
New Generation Glucose Hospital Meter System Ensures Accurate, Interference-Free and Safe Use
A new generation glucose hospital meter system now comes with several features that make hospital glucose testing easier and more secure while continuing to offer accuracy, freedom from interference, and... Read moreBusiness
view channel
Johnson & Johnson Acquires Cardiovascular Medical Device Company Shockwave Medical
Johnson & Johnson (New Brunswick, N.J., USA) and Shockwave Medical (Santa Clara, CA, USA) have entered into a definitive agreement under which Johnson & Johnson will acquire all of Shockwave’s... Read more