Mortality Rates Lower at Major Teaching Hospitals
|
By HospiMedica International staff writers Posted on 05 Jun 2017 |

Image: The Harvard School of Public Health (Photo courtesy of Wikimedia).
Admission to an academic medical center (AMC) is associated with a lower overall 30-day risk of death compared with admission to a non-teaching hospital, according to a new study.
Researchers at Harvard School of Public Health (HSPH; Boston, MA, USA), Massachusetts General Hospital (MGH; Boston, USA), and other institutions conducted a study using U.S. national Medicare data to compare mortality rates in teaching and non-teaching hospitals for common medical and surgical conditions among beneficiaries 65 years and older. The sample consisted of 21,451,824 total hospitalizations at 4,483 hospitals, of which 250 (5.6%) were major teaching, 894 (19.9%) were minor teaching, and 3,339 (74.3%) were non-teaching hospitals.
The main outcomes and measures were 30-day mortality rate for all hospitalizations and for 15 common medical and 6 surgical conditions. Secondary outcomes included 30-day mortality stratified by hospital size, and 7-day mortality and 90-day mortality for all hospitalizations, as well as for individual medical and surgical conditions. The results revealed that unadjusted 30-day mortality was 8.1% at major teaching hospitals, 9.2% at minor teaching hospitals, and 9.6% at non-teaching hospitals, representing a 1.5% mortality difference between major teaching hospitals and non-teaching hospitals.
After adjusting for patient and hospital characteristics, the same pattern persisted, but the difference in mortality between major and non-teaching hospitals was smaller. Further stratification by hospital size showed that 187 large (over 400 beds) AMCs had lower adjusted overall 30-day mortality (8.1%) relative to 76 large non-teaching hospitals (9.4%). The same pattern was observed in medium-sized hospitals. Among smaller hospitals, with less than 100 beds hospitals, minor teaching hospitals had lower overall 30-day mortality relative to non-teaching hospitals. The study was published on May 23, 2017, in JAMA.
“Academic medical centers provide a unique environment, with 24-hour availability of specialty services, advanced technologies, and some of the most expert physicians in the country. This seems to pay off for patients,” said lead author Laura Burke, MD, of HSPS. “While obviously not all patients can receive care in major teaching hospitals, understanding which strategies and resources are particularly important to patient outcomes, and how they can be replicated among nonteaching hospitals, is critically important to improve care for all patients.”
“We found to our surprise that across a wide range of medical and surgical conditions, patients at teaching hospitals did better; they were less likely to die,” added senior author Ashish Jha, MD, MPH, of HSPS. “While mortality may not be the only indicator that matters, it certainly is the most important one. We know that short term mortality is driven largely by how well the hospital does in taking care of patients.”
AMCs are often considered more expensive than community hospitals and some insurers have excluded them from their networks in an attempt to control costs, assuming that quality is comparable.
Related Links
Harvard School of Public Health
Massachusetts General Hospital
Researchers at Harvard School of Public Health (HSPH; Boston, MA, USA), Massachusetts General Hospital (MGH; Boston, USA), and other institutions conducted a study using U.S. national Medicare data to compare mortality rates in teaching and non-teaching hospitals for common medical and surgical conditions among beneficiaries 65 years and older. The sample consisted of 21,451,824 total hospitalizations at 4,483 hospitals, of which 250 (5.6%) were major teaching, 894 (19.9%) were minor teaching, and 3,339 (74.3%) were non-teaching hospitals.
The main outcomes and measures were 30-day mortality rate for all hospitalizations and for 15 common medical and 6 surgical conditions. Secondary outcomes included 30-day mortality stratified by hospital size, and 7-day mortality and 90-day mortality for all hospitalizations, as well as for individual medical and surgical conditions. The results revealed that unadjusted 30-day mortality was 8.1% at major teaching hospitals, 9.2% at minor teaching hospitals, and 9.6% at non-teaching hospitals, representing a 1.5% mortality difference between major teaching hospitals and non-teaching hospitals.
After adjusting for patient and hospital characteristics, the same pattern persisted, but the difference in mortality between major and non-teaching hospitals was smaller. Further stratification by hospital size showed that 187 large (over 400 beds) AMCs had lower adjusted overall 30-day mortality (8.1%) relative to 76 large non-teaching hospitals (9.4%). The same pattern was observed in medium-sized hospitals. Among smaller hospitals, with less than 100 beds hospitals, minor teaching hospitals had lower overall 30-day mortality relative to non-teaching hospitals. The study was published on May 23, 2017, in JAMA.
“Academic medical centers provide a unique environment, with 24-hour availability of specialty services, advanced technologies, and some of the most expert physicians in the country. This seems to pay off for patients,” said lead author Laura Burke, MD, of HSPS. “While obviously not all patients can receive care in major teaching hospitals, understanding which strategies and resources are particularly important to patient outcomes, and how they can be replicated among nonteaching hospitals, is critically important to improve care for all patients.”
“We found to our surprise that across a wide range of medical and surgical conditions, patients at teaching hospitals did better; they were less likely to die,” added senior author Ashish Jha, MD, MPH, of HSPS. “While mortality may not be the only indicator that matters, it certainly is the most important one. We know that short term mortality is driven largely by how well the hospital does in taking care of patients.”
AMCs are often considered more expensive than community hospitals and some insurers have excluded them from their networks in an attempt to control costs, assuming that quality is comparable.
Related Links
Harvard School of Public Health
Massachusetts General Hospital
Latest Hospital News News
- Nurse Tracking System Improves Hospital Workflow
- New Children’s Hospital Transforms California Healthcare
- Noisy Hospitals Face Threat of Decreased Federal Compensation
- Orthopedics Centre of Excellence Planned for Guy’s Hospital
- Research Suggests Avoidance of Low-Value Surgical Procedures
- U.S. Federal Readmission Fines Linked to Higher Mortality
- Columbia China to Build New Hospital in Jiaxing
- Dubai Debuts Second Robotic Pharmacy Service
- Seattle Hospital Network Shifts Away from Overlapping Surgeries
- ACC to Launch Valvular Heart Disease Program in China
- South Australia to Inaugurate Upscale Hospital
- Raffles to Launch Second Hospital Project in China
- Research Center Tackles Antimicrobial Drugs Challenge
- Miami Cardiac & Vascular Institute Completes Expansion Project
- Hospital Antibiotic Policies Improve Prescription Practices
- USC Virtual Care Clinic to Employ Avatar Doctors
Channels
Critical Care
view channel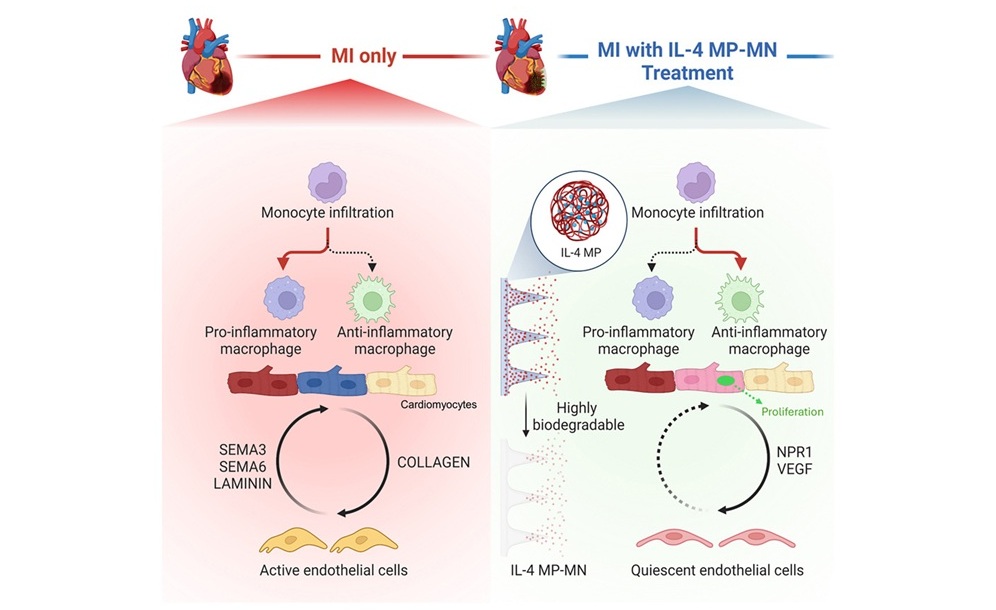
Biodegradable Patch Repairs Damaged Tissue After Heart Attack
A heart attack causes sudden loss of oxygen to the heart muscle, triggering cell death and a strong inflammatory response that often leads to scar formation. While scarring helps stabilize the heart, it... Read more
Magnetically Guided Microrobots to Enable Targeted Drug Delivery
Stroke affects 12 million people globally each year, often causing death or lasting disability. Current treatment relies on systemic administration of clot-dissolving drugs, which circulate throughout... Read more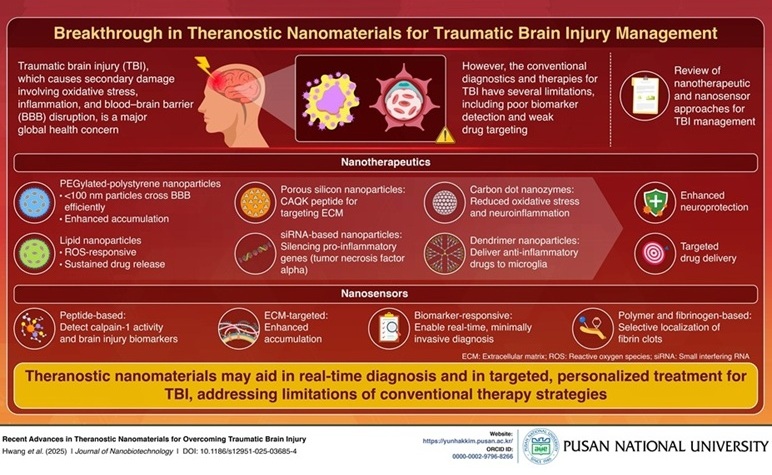
Smart Nanomaterials Detect and Treat Traumatic Brain Injuries Simultaneously
Traumatic brain injury (TBI) continues to leave millions with long-term disabilities every year. After a sudden impact from a fall, collision, or accident, the brain undergoes inflammation, oxidative stress,... Read more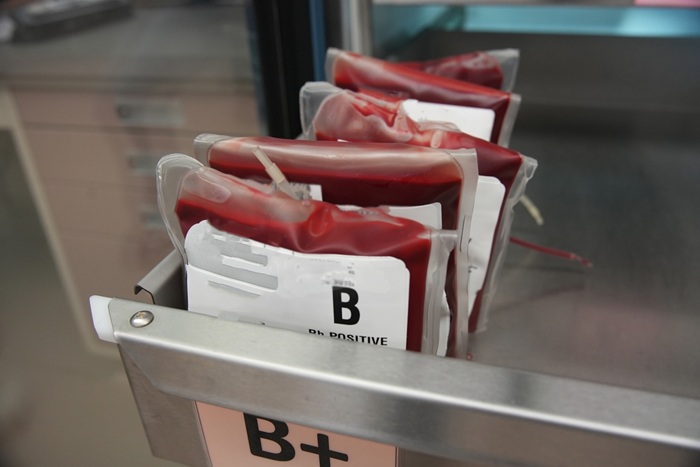
Earlier Blood Transfusion Could Reduce Heart Failure and Arrhythmia in Heart Disease Patients
Blood loss during or after surgery can place significant stress on people with heart disease, increasing the risk of dangerous complications. Transfusions are often delayed until hemoglobin levels fall... Read moreSurgical Techniques
view channelNovel Endoscopy Technique Provides Access to Deep Lung Tumors
Detecting lung cancer early can save lives, but diagnosing small tumors deep in the outer regions of the lungs remains a major clinical challenge. Although CT scans frequently identify tiny suspicious... Read more
New Study Findings Could Halve Number of Stent Procedures
When a coronary artery becomes acutely blocked during a heart attack, opening it immediately is essential to prevent irreversible damage. However, many patients also have other narrowed vessels that appear... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more