Night Shift Work Raises Diabetes Risk in Women
|
By HospiMedica International staff writers Posted on 02 Jan 2012 |
A new study has found that women who worked a rotating night shift had an increased risk of diabetes, a result that was not completely explained by an increase in body mass index (BMI).
Researchers at Brigham and Women's Hospital/Harvard School of Medicine (Boston, MD, USA) followed 69,269 women (aged 42-67) participating in the Nurses' Health Study I (NHS I) and 107,915 women (aged 25-42) enrolled in NHS II who were without diabetes, cardiovascular (CV) disease, or cancer at baseline. The participants were asked how long they had worked rotating night shifts--defined as at least three nights per month in addition to days and evenings in that month--at baseline; this information was updated every 2 to 4 years in NHS II. Self-reported type 2 diabetes was confirmed by a validated supplementary questionnaire.
In all, the researchers documented 6,165 (NHS I) and 3,961 (NHS II) incident type 2 diabetes cases during the 18-20 years of follow-up. On analysis, with adjustment for diabetes risk factors, the duration of shift work was monotonically associated with an increased risk of type 2 diabetes in both cohorts. Compared with women who reported no shift work, the pooled hazard ratio (HR) for participants with 1–2, 3–9, 10–19, and over 20 years of shift work were 1.05, 1.20, 1.40, and 1.58, respectively. Further adjustment for updated BMI attenuated the association, and the pooled hazard ratios were 1.03, 1.06, 1.10, and 1.24, respectively. The study was published on December 6, 2011, in PLoS Medicine.
“Rotating night shift work is generally associated with chronic misalignment between the endogenous circadian timing system and the behavior cycles,” explained senior author Frank Hu, MD, PhD, and colleagues of the department of nutrition. “This circadian misalignment has been found to result in adverse metabolic and cardiovascular consequences, including a decrease in leptin, an increase in glucose and insulin, an increase in mean arterial blood pressure, and reduced sleep efficiency.”
“Other factors such as disturbed sociotemporal patterns (resulting from atypical work hours leading to family problems, reduced social support, and stress) and unfavorable changes to biomarkers (e.g., cholesterol and other lipids, plasminogen, blood pressure, and cardiac activity) might also impact the association,” added the researchers.
Related Links:
Brigham and Women's Hospital/Harvard School of Medicine
Researchers at Brigham and Women's Hospital/Harvard School of Medicine (Boston, MD, USA) followed 69,269 women (aged 42-67) participating in the Nurses' Health Study I (NHS I) and 107,915 women (aged 25-42) enrolled in NHS II who were without diabetes, cardiovascular (CV) disease, or cancer at baseline. The participants were asked how long they had worked rotating night shifts--defined as at least three nights per month in addition to days and evenings in that month--at baseline; this information was updated every 2 to 4 years in NHS II. Self-reported type 2 diabetes was confirmed by a validated supplementary questionnaire.
In all, the researchers documented 6,165 (NHS I) and 3,961 (NHS II) incident type 2 diabetes cases during the 18-20 years of follow-up. On analysis, with adjustment for diabetes risk factors, the duration of shift work was monotonically associated with an increased risk of type 2 diabetes in both cohorts. Compared with women who reported no shift work, the pooled hazard ratio (HR) for participants with 1–2, 3–9, 10–19, and over 20 years of shift work were 1.05, 1.20, 1.40, and 1.58, respectively. Further adjustment for updated BMI attenuated the association, and the pooled hazard ratios were 1.03, 1.06, 1.10, and 1.24, respectively. The study was published on December 6, 2011, in PLoS Medicine.
“Rotating night shift work is generally associated with chronic misalignment between the endogenous circadian timing system and the behavior cycles,” explained senior author Frank Hu, MD, PhD, and colleagues of the department of nutrition. “This circadian misalignment has been found to result in adverse metabolic and cardiovascular consequences, including a decrease in leptin, an increase in glucose and insulin, an increase in mean arterial blood pressure, and reduced sleep efficiency.”
“Other factors such as disturbed sociotemporal patterns (resulting from atypical work hours leading to family problems, reduced social support, and stress) and unfavorable changes to biomarkers (e.g., cholesterol and other lipids, plasminogen, blood pressure, and cardiac activity) might also impact the association,” added the researchers.
Related Links:
Brigham and Women's Hospital/Harvard School of Medicine
Latest Patient Care News
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization

- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- Next Gen ICU Bed to Help Address Complex Critical Care Needs
- Groundbreaking AI-Powered UV-C Disinfection Technology Redefines Infection Control Landscape
- Clean Hospitals Can Reduce Antibiotic Resistance, Save Lives
- Smart Hospital Beds Improve Accuracy of Medical Diagnosis
- New Fast Endoscope Drying System Improves Productivity and Traceability
- World’s First Automated Endoscope Cleaner Fights Antimicrobial Resistance
- Portable High-Capacity Digital Stretcher Scales Provide Precision Weighing for Patients in ER
- Portable Clinical Scale with Remote Indicator Allows for Flexible Patient Weighing Use
- Innovative and Highly Customizable Medical Carts Offer Unlimited Configuration Possibilities
- Biomolecular Wound Healing Film Adheres to Sensitive Tissue and Releases Active Ingredients
- Wearable Health Tech Could Measure Gases Released From Skin to Monitor Metabolic Diseases
- Wearable Cardioverter Defibrillator System Protects Patients at Risk of Sudden Cardiac Arrest
Channels
Critical Care
view channel
Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
Intestinal gases are associated with several health conditions, including colon cancer, irritable bowel syndrome, and inflammatory bowel disease, and they have the potential to serve as crucial biomarkers... Read moreNovel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
Multiphoton microscopy has become an invaluable tool in neuroscience, allowing researchers to observe brain activity in real time with high-resolution imaging. A crucial aspect of many multiphoton microscopy... Read more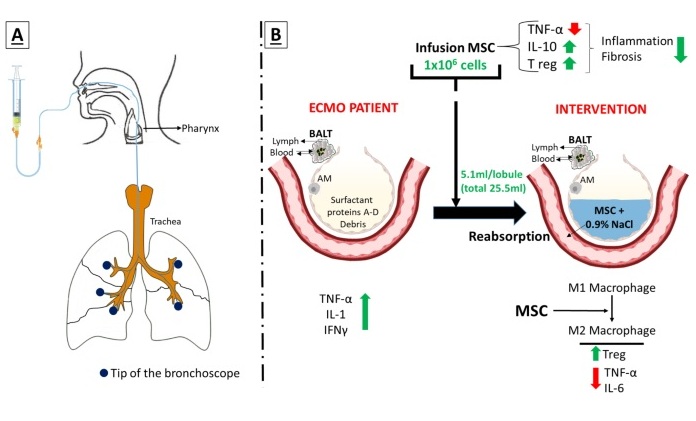
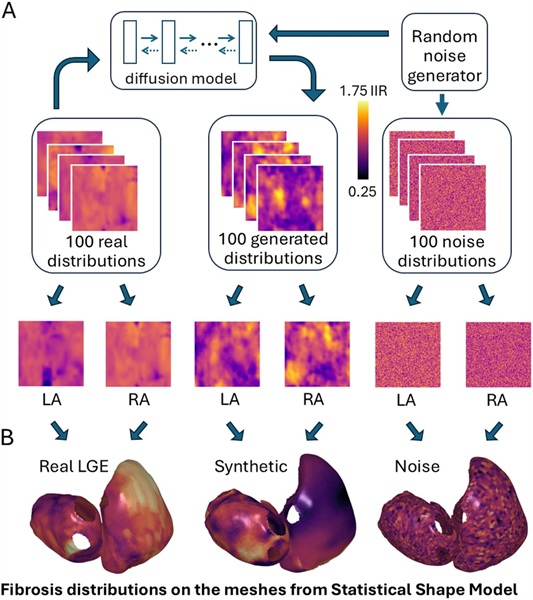
Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
Until now, administering cell therapies to patients on extracorporeal membrane oxygenation (ECMO)—a life-support system typically used for severe lung failure—has been nearly impossible.... Read moreSurgical Techniques
view channel
Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
In patients with coronary artery disease, certain blood vessels may be narrowed or blocked, requiring a stent or a bypass (also known as diversion) to restore blood flow to the heart. Bypass surgeries... Read more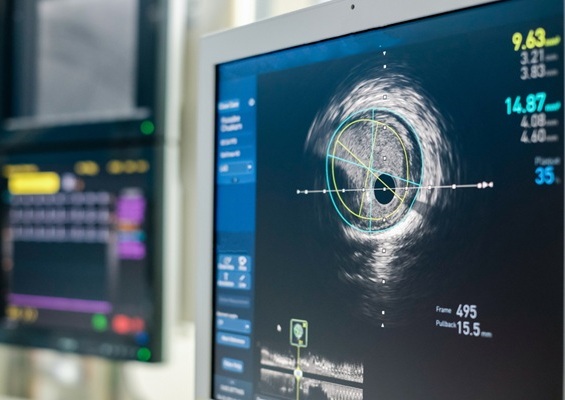
Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
Patients diagnosed with coronary artery disease, which is caused by plaque accumulation within the arteries leading to chest pain, shortness of breath, and potential heart attacks, frequently undergo percutaneous... Read more
World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
Surgeons have always faced challenges in measuring their progress toward surgical goals during procedures. Traditionally, obtaining measurements required stepping out of the sterile environment to perform... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more