Suboptimal Weight Affects Survival in Cervical Cancer
|
By HospiMedica International staff writers Posted on 05 May 2016 |
Both overweight and underweight women with cervical cancer did not live as long as their normal-weight counterparts, according to a new study.
Researchers at the University of Cincinnati (OH, USA) and the University of North Carolina (UNC; Chapel Hill, USA) conducted a retrospective cohort study of 623 women with cervical cancer treated from July 2000 to March 2013, classifying the women according to their body mass index (BMI). In all, 4% of the women were underweight, 30% were normal weight, and 66% were overweight or obese. The primary outcome was overall survival; secondary outcomes included stage, histopathology, disease-specific survival (DSS), and recurrence free survival (RFS).
The results showed that the median overall survival time in overweight or obese women was six months shorter than in women of normal weight (22 versus 28 months); for underweight women, median overall survival time was cut in half (14 versus 28 months). There was no difference in age, stage at presentation, grade, or histology between weight categories. After controlling for prognostic factors, underweight and overweight/obese patients had worse median RFS than normal weight patients. The study was published on April 14, 2016, in in Gynecologic Oncology.
“In understanding the effect of BMI on cervical cancer outcomes, it is important to recognize that both extremes of weight appear to negatively impact survival. A potential unifying hypothesis connecting both extremes of weight to poor cancer prognosis is chronic systemic inflammation,” wrote lead author Leslie Clark, MD, of UNC, and colleagues. “Both patients with cancer cachexia/sarcopenia and overweight/obese patients are in a heightened inflammatory state, which may lead to increased cell proliferation and inhibition of apoptosis.”
"However, this is likely not the only mechanism of poor outcomes. Co-morbid medical conditions might account for some of the differences in survival, particularly in morbidly obese patients,” concluded the authors. “Providers should optimize weight in underweight and overweight/obese patients to attempt to improve outcomes in these women. Interventions that target nutritional counseling and physical activity should be explored in these populations.”
Related Links:
University of Cincinnati
University of North Carolina
Researchers at the University of Cincinnati (OH, USA) and the University of North Carolina (UNC; Chapel Hill, USA) conducted a retrospective cohort study of 623 women with cervical cancer treated from July 2000 to March 2013, classifying the women according to their body mass index (BMI). In all, 4% of the women were underweight, 30% were normal weight, and 66% were overweight or obese. The primary outcome was overall survival; secondary outcomes included stage, histopathology, disease-specific survival (DSS), and recurrence free survival (RFS).
The results showed that the median overall survival time in overweight or obese women was six months shorter than in women of normal weight (22 versus 28 months); for underweight women, median overall survival time was cut in half (14 versus 28 months). There was no difference in age, stage at presentation, grade, or histology between weight categories. After controlling for prognostic factors, underweight and overweight/obese patients had worse median RFS than normal weight patients. The study was published on April 14, 2016, in in Gynecologic Oncology.
“In understanding the effect of BMI on cervical cancer outcomes, it is important to recognize that both extremes of weight appear to negatively impact survival. A potential unifying hypothesis connecting both extremes of weight to poor cancer prognosis is chronic systemic inflammation,” wrote lead author Leslie Clark, MD, of UNC, and colleagues. “Both patients with cancer cachexia/sarcopenia and overweight/obese patients are in a heightened inflammatory state, which may lead to increased cell proliferation and inhibition of apoptosis.”
"However, this is likely not the only mechanism of poor outcomes. Co-morbid medical conditions might account for some of the differences in survival, particularly in morbidly obese patients,” concluded the authors. “Providers should optimize weight in underweight and overweight/obese patients to attempt to improve outcomes in these women. Interventions that target nutritional counseling and physical activity should be explored in these populations.”
Related Links:
University of Cincinnati
University of North Carolina
Latest Patient Care News
- Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
- VR Training Tool Combats Contamination of Portable Medical Equipment
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization

- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- Next Gen ICU Bed to Help Address Complex Critical Care Needs
- Groundbreaking AI-Powered UV-C Disinfection Technology Redefines Infection Control Landscape
- Clean Hospitals Can Reduce Antibiotic Resistance, Save Lives
- Smart Hospital Beds Improve Accuracy of Medical Diagnosis
- New Fast Endoscope Drying System Improves Productivity and Traceability
- World’s First Automated Endoscope Cleaner Fights Antimicrobial Resistance
- Portable High-Capacity Digital Stretcher Scales Provide Precision Weighing for Patients in ER
- Portable Clinical Scale with Remote Indicator Allows for Flexible Patient Weighing Use
- Innovative and Highly Customizable Medical Carts Offer Unlimited Configuration Possibilities
- Biomolecular Wound Healing Film Adheres to Sensitive Tissue and Releases Active Ingredients
Channels
Artificial Intelligence
view channelCritical Care
view channel
AI Stethoscope Spots Heart Valve Disease Earlier Than GPs
Valvular heart disease affects more than half of people over 65, yet it often goes undiagnosed until symptoms become severe. In advanced stages, untreated cases can carry a mortality risk of up to 80%... Read more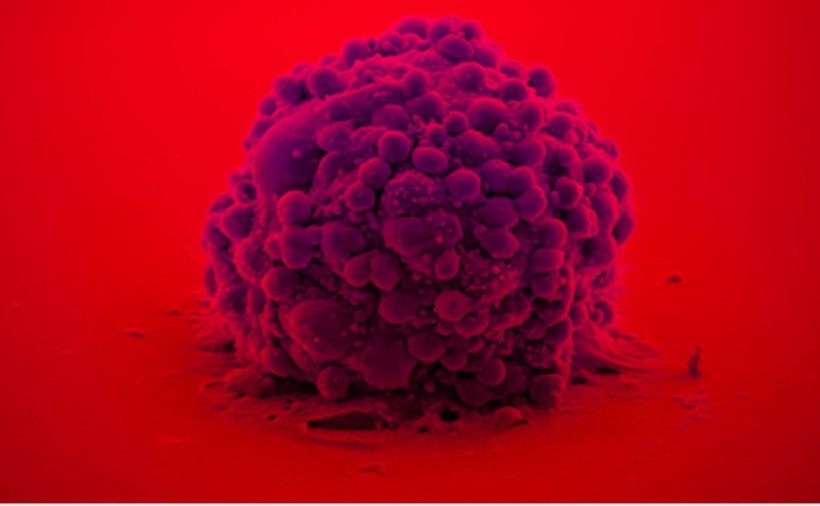
Bioadhesive Patch Eliminates Cancer Cells That Remain After Brain Tumor Surgery
Glioblastoma is the most common and aggressive form of brain tumor, characterized by rapid growth, high invasiveness, and an extremely poor prognosis. Even with surgery followed by radiotherapy and chemotherapy,... Read moreSurgical Techniques
view channel
Surgical Innovation Cuts Ovarian Cancer Risk by 80%
Ovarian cancer remains the deadliest gynecological cancer, largely because there is no reliable screening test, and most cases are diagnosed at advanced stages. Thousands of patients die each year as treatment... Read more
New Imaging Combo Offers Hope for High-Risk Heart Patients
Patients with type 2 diabetes often develop complex, severe coronary artery disease involving multiple narrowed or blocked arteries, making complete revascularization difficult. Without detailed functional... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more