Combination Labor Induction Method Shortens Delivery Time
|
By HospiMedica International staff writers Posted on 15 Dec 2016 |
A combination of mechanical and pharmacologic labor induction leads to delivery several hours earlier than either method alone, claims a new study.
Researchers at the University of Pennsylvania (PA, USA) conducted a randomized trial to compare four labor induction methods: misoprostol (a prostaglandin-like drug) alone, cervical Foley catheter alone, concurrent use of misoprostol and a cervical Foley catheter, and concurrent use of a Foley catheter and the contraction-inducing hormone oxytocin. In all, from May 2013 to June 2015, 491 women undergoing labor induction with full-term singleton, vertex-presenting gestations, and no contraindication to vaginal delivery participated, with the primary outcome being time to delivery.
The results showed the average time between treatment and delivery was lowest for the misoprostol-Foley combination at 13.1 hours, compared to 14.5 hours for Foley-oxytocin, 17.6 hours for misoprostol alone, and 17.7 hours for the Foley method alone. According to the researchers, the more than four-hour gap between misoprostol-Foley and either method alone is clinically meaningful, particularly considering that the various methods did not produce significant differences in the rates of cesarean deliveries or of serious medical complications for the mother or child. The study was published in the December 2016 issue of Obstetrics & Gynecology.
"Using combination methods in every case of labor induction in America would spare pregnant women more than 100,000 days of labor annually,” said lead author Lisa Levine, MD. “That in turn would reduce hospital costs, reduce the health risks to mother and child that come with prolonged labor, and reduce the stress that mothers experience while awaiting delivery.”
Labor induction is one of the most common medical procedures in the world, with nearly one million women who deliver in the United States alone undergoing the procedure annually. But despite its widespread use, including for medical conditions such as preeclampsia, gestational diabetes, or other health risks to the mother or baby, labor induction is still costly and has no widely accepted best practice guideline.
Related Links:
University of Pennsylvania
Researchers at the University of Pennsylvania (PA, USA) conducted a randomized trial to compare four labor induction methods: misoprostol (a prostaglandin-like drug) alone, cervical Foley catheter alone, concurrent use of misoprostol and a cervical Foley catheter, and concurrent use of a Foley catheter and the contraction-inducing hormone oxytocin. In all, from May 2013 to June 2015, 491 women undergoing labor induction with full-term singleton, vertex-presenting gestations, and no contraindication to vaginal delivery participated, with the primary outcome being time to delivery.
The results showed the average time between treatment and delivery was lowest for the misoprostol-Foley combination at 13.1 hours, compared to 14.5 hours for Foley-oxytocin, 17.6 hours for misoprostol alone, and 17.7 hours for the Foley method alone. According to the researchers, the more than four-hour gap between misoprostol-Foley and either method alone is clinically meaningful, particularly considering that the various methods did not produce significant differences in the rates of cesarean deliveries or of serious medical complications for the mother or child. The study was published in the December 2016 issue of Obstetrics & Gynecology.
"Using combination methods in every case of labor induction in America would spare pregnant women more than 100,000 days of labor annually,” said lead author Lisa Levine, MD. “That in turn would reduce hospital costs, reduce the health risks to mother and child that come with prolonged labor, and reduce the stress that mothers experience while awaiting delivery.”
Labor induction is one of the most common medical procedures in the world, with nearly one million women who deliver in the United States alone undergoing the procedure annually. But despite its widespread use, including for medical conditions such as preeclampsia, gestational diabetes, or other health risks to the mother or baby, labor induction is still costly and has no widely accepted best practice guideline.
Related Links:
University of Pennsylvania
Latest Patient Care News
- Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
- VR Training Tool Combats Contamination of Portable Medical Equipment
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization

- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- Next Gen ICU Bed to Help Address Complex Critical Care Needs
- Groundbreaking AI-Powered UV-C Disinfection Technology Redefines Infection Control Landscape
- Clean Hospitals Can Reduce Antibiotic Resistance, Save Lives
- Smart Hospital Beds Improve Accuracy of Medical Diagnosis
- New Fast Endoscope Drying System Improves Productivity and Traceability
- World’s First Automated Endoscope Cleaner Fights Antimicrobial Resistance
- Portable High-Capacity Digital Stretcher Scales Provide Precision Weighing for Patients in ER
- Portable Clinical Scale with Remote Indicator Allows for Flexible Patient Weighing Use
- Innovative and Highly Customizable Medical Carts Offer Unlimited Configuration Possibilities
- Biomolecular Wound Healing Film Adheres to Sensitive Tissue and Releases Active Ingredients
Channels
Critical Care
view channel
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read more
'Universal' Kidney to Match Any Blood Type
Blood-type incompatibility has long been one of the greatest obstacles in organ transplantation, forcing thousands of patients—particularly those with type O blood—to wait years longer for compatible donors.... Read moreSurgical Techniques
view channel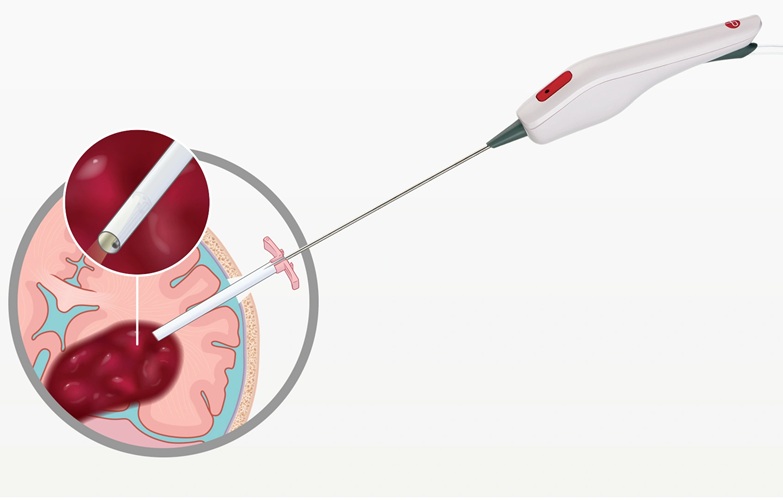
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read more
Novel Glue Prevents Complications After Breast Cancer Surgery
Seroma and prolonged lymphorrhea are among the most common complications following axillary lymphadenectomy in breast cancer patients. These postoperative issues can delay recovery and postpone the start... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more