Second Opinions Reveal Extent of Diagnostic Error
|
By HospiMedica International staff writers Posted on 20 Apr 2017 |
A new study reports that as many as 88% of patients referred for a second opinion receive a refined diagnosis that can change their care plan, and potentially their lives.
Researchers at the Mayo Clinic conducted a retrospective study of 286 patients referred for additional consultation by physicians, physician assistants, and nurse practitioners from primary care practices from January 1, 2009 to December 31, 2010. Patients' referral and final diagnoses were compared and classified into one of three categories: equal referral diagnosis and final diagnosis, referral diagnosis better defined or refined, and referral diagnosis distinctly different from final diagnosis.
The results revealed that in 12% of cases, referral diagnoses were the same as the final diagnoses. Final diagnoses were better defined or more refined in 66% of the cases; but in 21% of cases, the final diagnoses were distinctly different than the referral diagnoses. The researchers also identified costs associated with second opinions, and found that total diagnostic costs for cases resulting in a different final diagnosis were significantly higher than those for confirmed or refined diagnoses. The study was published on April 4, 2017, in Journal of Evaluation in Clinical Practice.
“Effective and efficient treatment depends on the right diagnosis. Referrals to advanced specialty care for undifferentiated problems are an essential component of patient care,” said lead author health care policy researcher James Naessens, ScD. “Knowing that more than one out of every five referral patients may be completely [and] incorrectly diagnosed is troubling, not only because of the safety risks for these patients prior to correct diagnosis, but also because of the patients we assume are not being referred at all.”
Diagnostic uncertainty is often encountered in a medical practice. Patients with ambiguous, uncertain, and undiagnosed problems are frequently referred for second opinions. But in order to reduce costs, health insurers often limit access to care outside their own network, effectively limiting referrals. In addition, primary care providers may be more confident in their diagnostic expertise than warranted in a particular case, or patients may lack the knowledge or assertiveness to request a referral.
Researchers at the Mayo Clinic conducted a retrospective study of 286 patients referred for additional consultation by physicians, physician assistants, and nurse practitioners from primary care practices from January 1, 2009 to December 31, 2010. Patients' referral and final diagnoses were compared and classified into one of three categories: equal referral diagnosis and final diagnosis, referral diagnosis better defined or refined, and referral diagnosis distinctly different from final diagnosis.
The results revealed that in 12% of cases, referral diagnoses were the same as the final diagnoses. Final diagnoses were better defined or more refined in 66% of the cases; but in 21% of cases, the final diagnoses were distinctly different than the referral diagnoses. The researchers also identified costs associated with second opinions, and found that total diagnostic costs for cases resulting in a different final diagnosis were significantly higher than those for confirmed or refined diagnoses. The study was published on April 4, 2017, in Journal of Evaluation in Clinical Practice.
“Effective and efficient treatment depends on the right diagnosis. Referrals to advanced specialty care for undifferentiated problems are an essential component of patient care,” said lead author health care policy researcher James Naessens, ScD. “Knowing that more than one out of every five referral patients may be completely [and] incorrectly diagnosed is troubling, not only because of the safety risks for these patients prior to correct diagnosis, but also because of the patients we assume are not being referred at all.”
Diagnostic uncertainty is often encountered in a medical practice. Patients with ambiguous, uncertain, and undiagnosed problems are frequently referred for second opinions. But in order to reduce costs, health insurers often limit access to care outside their own network, effectively limiting referrals. In addition, primary care providers may be more confident in their diagnostic expertise than warranted in a particular case, or patients may lack the knowledge or assertiveness to request a referral.
Latest Patient Care News
- Portable Biosensor Platform to Reduce Hospital-Acquired Infections
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization

- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- Next Gen ICU Bed to Help Address Complex Critical Care Needs
- Groundbreaking AI-Powered UV-C Disinfection Technology Redefines Infection Control Landscape
- Clean Hospitals Can Reduce Antibiotic Resistance, Save Lives
- Smart Hospital Beds Improve Accuracy of Medical Diagnosis
- New Fast Endoscope Drying System Improves Productivity and Traceability
- World’s First Automated Endoscope Cleaner Fights Antimicrobial Resistance
- Portable High-Capacity Digital Stretcher Scales Provide Precision Weighing for Patients in ER
- Portable Clinical Scale with Remote Indicator Allows for Flexible Patient Weighing Use
- Innovative and Highly Customizable Medical Carts Offer Unlimited Configuration Possibilities
- Biomolecular Wound Healing Film Adheres to Sensitive Tissue and Releases Active Ingredients
- Wearable Health Tech Could Measure Gases Released From Skin to Monitor Metabolic Diseases
- Wearable Cardioverter Defibrillator System Protects Patients at Risk of Sudden Cardiac Arrest
Channels
Artificial Intelligence
view channel
Innovative Risk Score Predicts Heart Attack or Stroke in Kidney Transplant Candidates
Heart researchers have utilized an innovative risk assessment score to accurately predict whether patients being evaluated for kidney transplants are at risk for future major cardiac events, such as a... Read more
AI Algorithm Detects Early-Stage Metabolic-Associated Steatotic Liver Disease Using EHRs
Liver disease, which is treatable when detected early, often goes unnoticed until it reaches advanced stages. Metabolic-associated steatotic liver disease (MASLD), the most prevalent form of liver disease,... Read moreCritical Care
view channel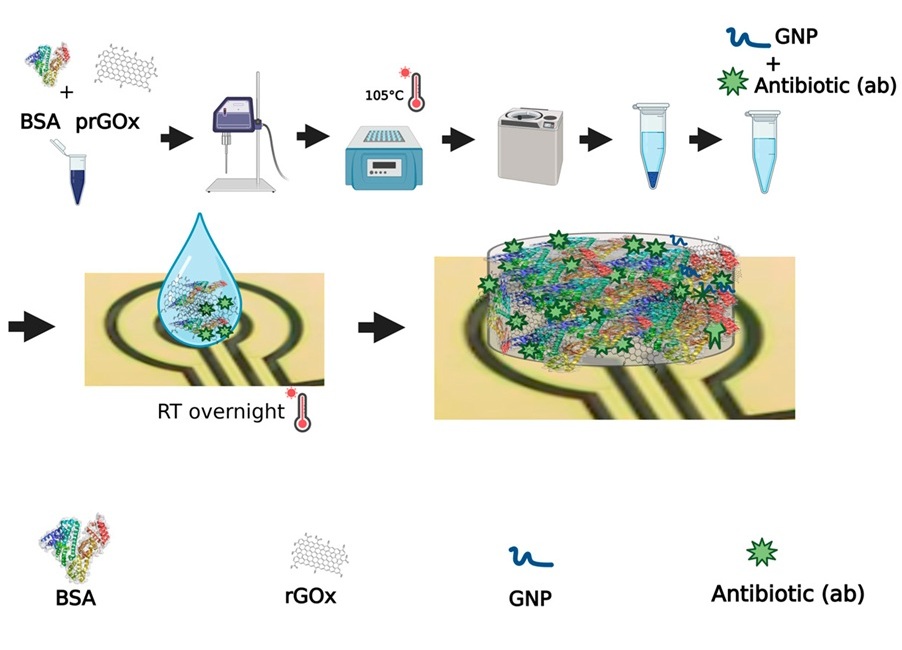
Novel Coating Significantly Extends Longevity of Implantable Biosensors
Wearable and implantable biosensors capable of accurately detecting biological molecules in a non-invasive or minimally invasive way offer enormous potential for monitoring patients’ health and their responses... Read more
Nanogel-Based Drug Delivery Technology to Improve UTI Treatment
Urinary tract infections (UTIs) are not only widespread and costly but also highly debilitating, significantly impacting the quality of life for those affected. The antibiotics commonly used to treat UTIs... Read more
New IV Pole Improves Safety and Ease of Administering IV Medications at Hospital Bedside
Preventable medication errors affect around 500,000 hospitalized patients in the U.S. every year. A significant portion of these errors occur with intravenous (IV) smart pumps, which require a precise... Read moreSurgical Techniques
view channel
Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
Surgical adhesions are a frequent and often life-threatening complication following open or laparoscopic abdominal surgery. These adhesions develop in the weeks following surgery as the body heals.... Read more
Groundbreaking Leadless Pacemaker to Prevent Invasive Surgeries for Children
Leadless pacemakers marked a significant advancement in cardiac care, primarily because traditional pacemakers are dependent on leads, which are prone to breakage over time. Currently, two FDA-approved... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read morePoint of Care
view channel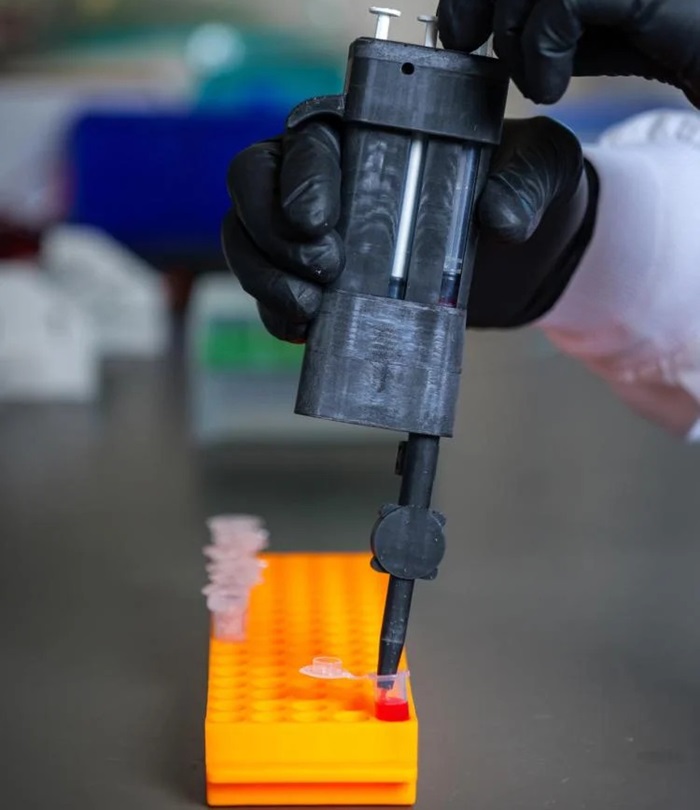
Handheld, Sound-Based Diagnostic System Delivers Bedside Blood Test Results in An Hour
Patients who go to a doctor for a blood test often have to contend with a needle and syringe, followed by a long wait—sometimes hours or even days—for lab results. Scientists have been working hard to... Read more
Smartphone-Enabled, Paper-Based Quantitative Diagnostic Platform Transforms POC Testing
Point-of-care diagnostics are crucial for public health, offering rapid, on-site testing that enables prompt diagnosis and treatment. This is especially valuable in remote or underserved regions where... Read moreBusiness
view channel
Becton Dickinson to Spin Out Biosciences and Diagnostic Solutions Business
Becton, Dickinson and Company (BD, Franklin Lakes, NJ, USA), has announced that its board of directors has unanimously authorized BD management to pursue a plan to separate BD's Biosciences and Diagnostic... Read more