New COVID-19 Test Detects Cell Mediated (T Cell) Immune Response to SARS-CoV-2 Infection
|
By HospiMedica International staff writers Posted on 08 Mar 2021 |

Image: T-SPOT.COVID test (Photo courtesy of Oxford Immunotec Global PLC)
A new COVID-19 test for the qualitative detection of a cell mediated (T cell) immune response to SARS-CoV-2 in human whole blood has just been launched.
Oxford Immunotec Global PLC (Oxford, UK) has launched the T-SPOT.COVID test, a CE marked ELISPOT based test intended for qualitative detection of a cell mediated (T cell) immune response to SARS-CoV-2 in human whole blood. The company developed the T-SPOT.COVID test as an evolution of its T-SPOT Discovery SARS-CoV-2 assay, a research use only test used to gain insights about the immune response to SARS-CoV-2. Oxford Immunotec has filed an EUA request to the FDA for the test.
Serology does not give the full picture of the adaptive immune response to SARS-CoV-2 infection. Antibodies are not always produced in response to SARS-CoV-2 infection, or may be delayed. Antibodies can also wane quickly after infection and reports show T cells may be more long lived than the antibody response. In the absence of an antibody response, the T cell response may be protective from SARS-CoV-2 infection.
In a clinical study using samples collected in the US, the T-SPOT.COVID test was proven to detect a SARS-CoV-2 cell mediated (T cell) immune response in PCR positive individuals, even with negative serology test results6. The T-SPOT.COVID test therefore, complements results obtained by antibody serology to give a more comprehensive view of an individual's adaptive immune response to SARS-CoV-2 infection. The test could also be used, for example, alongside serology tests to support clinical assessment of individuals who present with suspected COVID-19 but are PCR negative.
In the study, the T-SPOT.COVID test had a positive agreement with PCR-results of 96.6% (84/87) in SARS-CoV-2 infected individuals <60 days after first PCR positive result. At >60 days (with the furthest time point after first positive PCR test result being >240 days) positive agreement remained high at 83.3% (40/48). The T-SPOT.COVID test detected substantially more people with previous positive PCR results than serology in the cohort, whose positivity rate was lower and declined faster over time.
In an endemic cohort of US individuals selected to be at a relative lower risk of SARS-CoV-2 infection (based on the absence of self-reported symptoms, negative serology results and no prior history of a positive PCR test result for SARS-CoV-2) the T-SPOT.COVID test had a negative agreement of 98.0% (96/98). However, there is a possibility that a proportion of this group had, or still have, an asymptomatic infection, seronegative at the time of testing, but in whom the T-SPOT.COVID test was able to detect a T cell response.
"T cells and antibodies are two arms of the adaptive immune response. The detection and measurement of each can provide different insights about disease activity and an individual's personal immunity," said Phill Keefe, Senior VP, Product Design, Development and Delivery at Oxford Immunotec.
"The T-SPOT® Technology platform is a standardized way of measuring T cells. It has been proven in clinical use for over 18 years with another major infectious disease, tuberculosis, which kills around 1.5 million people every year," said Dr. Peter Wrighton-Smith, CEO of Oxford Immunotec. "Our T-SPOT.COVID test is tailored specifically for the detection and measurement of an individual's T cell response to SARS-CoV-2 infection. Having the ability to determine an individual's immune response to SARS-CoV-2 has the potential to support a wide range of needs in our battle against the COVID-19 pandemic."
Related Links:
Oxford Immunotec Global PLC
Oxford Immunotec Global PLC (Oxford, UK) has launched the T-SPOT.COVID test, a CE marked ELISPOT based test intended for qualitative detection of a cell mediated (T cell) immune response to SARS-CoV-2 in human whole blood. The company developed the T-SPOT.COVID test as an evolution of its T-SPOT Discovery SARS-CoV-2 assay, a research use only test used to gain insights about the immune response to SARS-CoV-2. Oxford Immunotec has filed an EUA request to the FDA for the test.
Serology does not give the full picture of the adaptive immune response to SARS-CoV-2 infection. Antibodies are not always produced in response to SARS-CoV-2 infection, or may be delayed. Antibodies can also wane quickly after infection and reports show T cells may be more long lived than the antibody response. In the absence of an antibody response, the T cell response may be protective from SARS-CoV-2 infection.
In a clinical study using samples collected in the US, the T-SPOT.COVID test was proven to detect a SARS-CoV-2 cell mediated (T cell) immune response in PCR positive individuals, even with negative serology test results6. The T-SPOT.COVID test therefore, complements results obtained by antibody serology to give a more comprehensive view of an individual's adaptive immune response to SARS-CoV-2 infection. The test could also be used, for example, alongside serology tests to support clinical assessment of individuals who present with suspected COVID-19 but are PCR negative.
In the study, the T-SPOT.COVID test had a positive agreement with PCR-results of 96.6% (84/87) in SARS-CoV-2 infected individuals <60 days after first PCR positive result. At >60 days (with the furthest time point after first positive PCR test result being >240 days) positive agreement remained high at 83.3% (40/48). The T-SPOT.COVID test detected substantially more people with previous positive PCR results than serology in the cohort, whose positivity rate was lower and declined faster over time.
In an endemic cohort of US individuals selected to be at a relative lower risk of SARS-CoV-2 infection (based on the absence of self-reported symptoms, negative serology results and no prior history of a positive PCR test result for SARS-CoV-2) the T-SPOT.COVID test had a negative agreement of 98.0% (96/98). However, there is a possibility that a proportion of this group had, or still have, an asymptomatic infection, seronegative at the time of testing, but in whom the T-SPOT.COVID test was able to detect a T cell response.
"T cells and antibodies are two arms of the adaptive immune response. The detection and measurement of each can provide different insights about disease activity and an individual's personal immunity," said Phill Keefe, Senior VP, Product Design, Development and Delivery at Oxford Immunotec.
"The T-SPOT® Technology platform is a standardized way of measuring T cells. It has been proven in clinical use for over 18 years with another major infectious disease, tuberculosis, which kills around 1.5 million people every year," said Dr. Peter Wrighton-Smith, CEO of Oxford Immunotec. "Our T-SPOT.COVID test is tailored specifically for the detection and measurement of an individual's T cell response to SARS-CoV-2 infection. Having the ability to determine an individual's immune response to SARS-CoV-2 has the potential to support a wide range of needs in our battle against the COVID-19 pandemic."
Related Links:
Oxford Immunotec Global PLC
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Critical Care
view channel_1.jpg)
Cutting-Edge Bioelectronic Device Offers Drug-Free Approach to Managing Bacterial Infections
Antibiotic-resistant infections pose an increasing threat to patient safety and healthcare systems worldwide. Recent estimates indicate that drug-resistant infections may rise by 70% by 2050, highlighting... Read more
Sophisticated Machine-Learning Approach Uses Patient EHRs to Predict Pneumonia Outcomes
Pneumonia, an infection that results in difficulty breathing due to fluid accumulation in the lungs, is one of the leading causes of death worldwide. This condition is particularly challenging to treat... Read more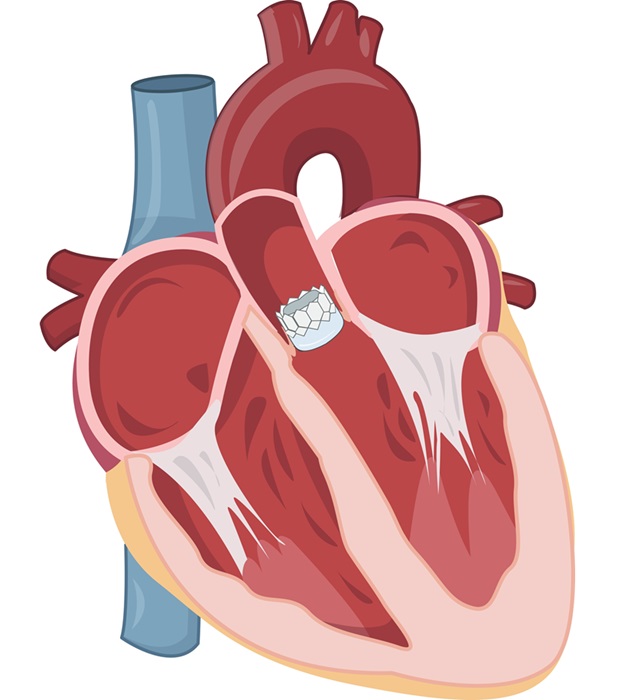
Early TAVR Benefits Patients with Asymptomatic Severe Aortic Stenosis
For patients with asymptomatic severe aortic stenosis (AS) and preserved left-ventricular ejection fraction, current guidelines recommend clinical surveillance every six to twelve months.... Read more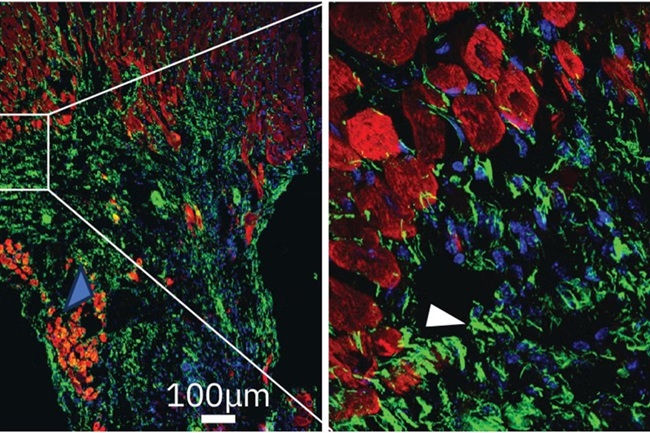
First-Of-Its-Kind Experimental Therapy Enhances Tissue Repair After Heart Attack
Cardiovascular disease remains the leading cause of death worldwide, accounting for one-third of all annual fatalities. Following a heart attack, the heart's natural regenerative ability is limited, resulting... Read moreSurgical Techniques
view channel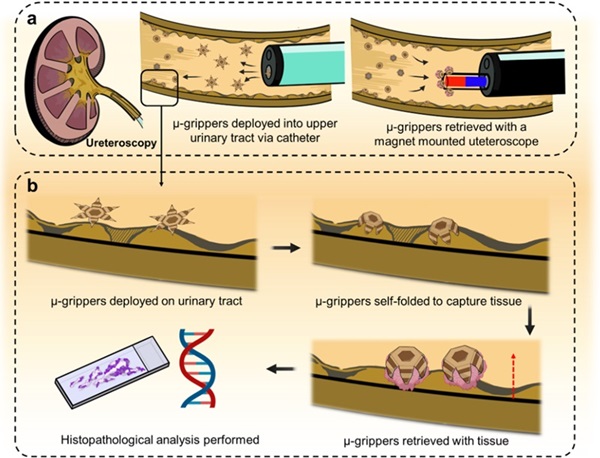
Microgrippers For Miniature Biopsies to Create New Cancer Diagnostic Screening Paradigm
The standard diagnosis of upper urinary tract cancers typically involves the removal of suspicious tissue using forceps, a procedure that is technically challenging and samples only a single region of the organ.... Read moreMiniature Soft Lithium-Ion Battery Could Be Used as Defibrillator During Surgery
The development of tiny smart devices, measuring just a few cubic millimeters, requires equally miniature power sources. For minimally invasive biomedical devices that interact with biological tissues,... Read more.jpg)
TAVI Procedure Supported by Radial Artery Access Reduces Bleeding Complications
The TAVI procedure, or Transcatheter Aortic Valve Implantation, is a minimally invasive technique in which a new aortic valve is inserted through a femoral artery to replace a narrowed old valve.... Read more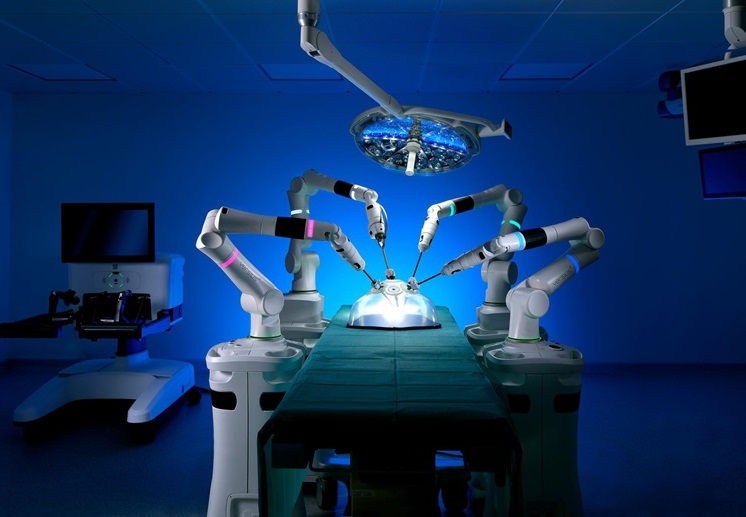
Portable Surgical Robot Seamlessly Integrates into Any OR for Performing Cholecystectomy Procedures
The United States represents a significant market with a strong demand for a flexible surgical robotic system applicable across various care settings. However, there has been a lack of sufficient options... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel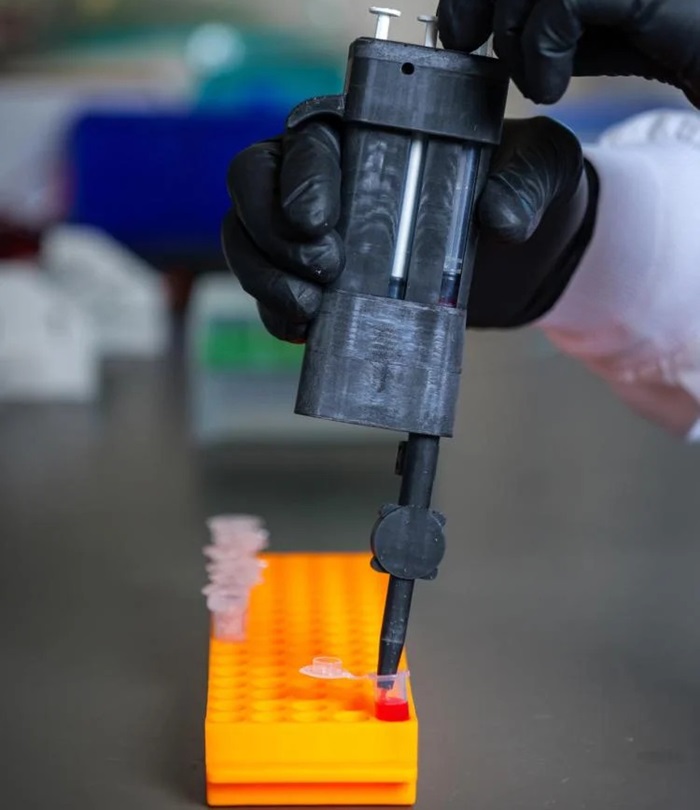
Handheld, Sound-Based Diagnostic System Delivers Bedside Blood Test Results in An Hour
Patients who go to a doctor for a blood test often have to contend with a needle and syringe, followed by a long wait—sometimes hours or even days—for lab results. Scientists have been working hard to... Read more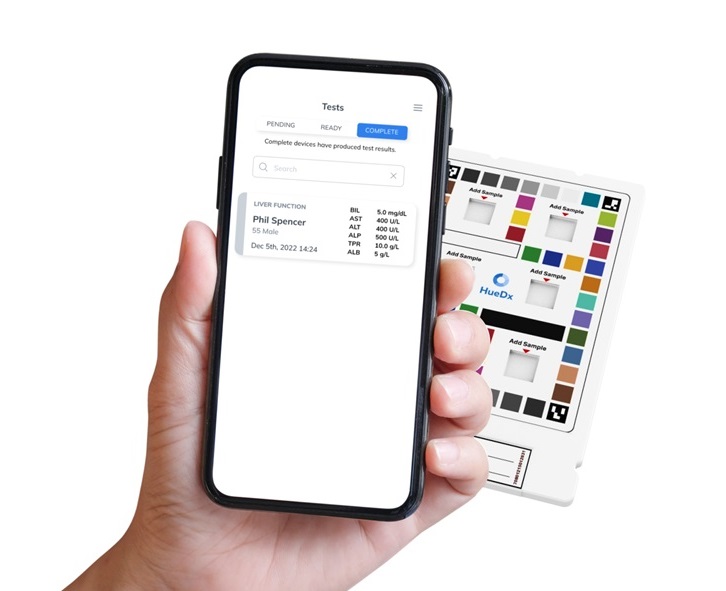
Smartphone-Enabled, Paper-Based Quantitative Diagnostic Platform Transforms POC Testing
Point-of-care diagnostics are crucial for public health, offering rapid, on-site testing that enables prompt diagnosis and treatment. This is especially valuable in remote or underserved regions where... Read moreBusiness
view channel
Hologic Acquires Gynesonics to Strengthen Existing Gynecological Surgical Business
Hologic (Marlborough, MA, USA) has signed a definitive agreement to acquire Gynesonics (Redwood City, CA, USA) for approximately USD 350 million, subject to working capital and other customary closing adjustments.... Read more