Point-of-Care Ultrasound Predicts Clinical Outcomes in Patients with COVID-19
|
By HospiMedica International staff writers Posted on 06 Sep 2021 |

Image: GE Healthcare Vscan (Photo courtesy of GE Healthcare)
Point-of-care ultrasound (POCUS) can detect the pulmonary manifestations of COVID-19 and predict patient outcomes, according to a new study.
These findings were from a prospective cohort study conducted by researchers of Stanford University (Stanford, CA, USA) at four hospitals from March 2020 to January 2021 to evaluate lung POCUS and clinical outcomes of COVID-19. Inclusion criteria included adult patients hospitalized for COVID-19 who received lung POCUS with a 12-zone protocol. Each image was interpreted by two reviewers blinded to clinical outcomes. The study’s primary outcome was the need for intensive care unit (ICU) admission versus no ICU admission. Secondary outcomes included intubation and supplemental oxygen usage.
POCUS has garnered substantial interest as a potential modality to expediently diagnose COVID-19 and its complications. POCUS devices are cheaper than traditional imaging equipment, such as X-ray or computed tomography (CT) machines, which makes POCUS ideal for surge scenarios and resource-limited settings. Since providers using POCUS are concomitantly at the bedside assessing patients, POCUS permits an immediate and augmented evaluation of the patient. It can reduce personal protective equipment usage by radiology technicians as well as the need to decontaminate larger radiographic equipment. POCUS has also been successfully used in the diagnosis and management of COVID-19. Previously described pulmonary manifestations of COVID-19 include pulmonary edema, lung consolidation, and pleural-line irregularities. POCUS can diagnose these pathological states with similar accuracy to CT and with higher sensitivity than X-ray.
Although lung ultrasound abnormalities are more common in patients who experience adverse outcomes with COVID-19, few studies have examined whether scans performed early in the hospitalization can provide meaningful risk stratification. Furthermore, few scoring tools predict the need for oxygen on discharge, which represents a limited resource in many settings. In the latest study, the researchers examined whether early pulmonary POCUS findings correlate with important clinical outcomes, such as intensive care admission or need for supplemental oxygen. They also examined whether these findings, if detected early, are predictive of future clinical outcomes in the subsequent hospital course or after discharge.
In this prospective cohort study conducted at four medical centers of patients hospitalized with COVID-19, the researchers found that lung ultrasounds collected within 24 hours of emergency department triage were predictive of important clinical outcomes in the subsequent hospital course, including ICU admission, intubation, supplemental oxygen usage, and the need for oxygen at discharge. Ultrasound findings associated with an adverse clinical course included B-lines and consolidations (particularly in the anterior and lateral lung fields), while a normal ultrasound on triage was protective against adverse outcomes. Notably, ultrasound findings did not dynamically change over a 28-day window after symptom onset, suggesting that the presence of B-lines or consolidations, regardless of when they are detected, may be important clinical predictors.
Previous investigations have demonstrated that lung POCUS findings (such as B-lines or consolidations) are associated with critical illness and intubation for COVID-19. The new study expands on these observations by demonstrating that scans collected within 24 hours of ED triage may predict outcomes for the entire hospital course, including future supplemental oxygen usage and the need for oxygen on discharge. This information may substantially aid frontline providers in resource-limited settings experiencing patient surges. In such scenarios, POCUS could augment admission or discharge decisions for providers. More broadly, POCUS could represent one of several tools to identify patients at-risk for adverse outcomes. Other authors have demonstrated the utility of laboratory tests (eg, ferritin, c-reactive protein) or radiographic findings for risk stratification. POCUS may have potential advantages over these other methods in that it is more expedient, low cost and does not expose the patient to ionizing radiation. Future studies are needed to directly compare POCUS with other scoring systems that utilize laboratory or radiological findings.
Related Links:
Stanford University
These findings were from a prospective cohort study conducted by researchers of Stanford University (Stanford, CA, USA) at four hospitals from March 2020 to January 2021 to evaluate lung POCUS and clinical outcomes of COVID-19. Inclusion criteria included adult patients hospitalized for COVID-19 who received lung POCUS with a 12-zone protocol. Each image was interpreted by two reviewers blinded to clinical outcomes. The study’s primary outcome was the need for intensive care unit (ICU) admission versus no ICU admission. Secondary outcomes included intubation and supplemental oxygen usage.
POCUS has garnered substantial interest as a potential modality to expediently diagnose COVID-19 and its complications. POCUS devices are cheaper than traditional imaging equipment, such as X-ray or computed tomography (CT) machines, which makes POCUS ideal for surge scenarios and resource-limited settings. Since providers using POCUS are concomitantly at the bedside assessing patients, POCUS permits an immediate and augmented evaluation of the patient. It can reduce personal protective equipment usage by radiology technicians as well as the need to decontaminate larger radiographic equipment. POCUS has also been successfully used in the diagnosis and management of COVID-19. Previously described pulmonary manifestations of COVID-19 include pulmonary edema, lung consolidation, and pleural-line irregularities. POCUS can diagnose these pathological states with similar accuracy to CT and with higher sensitivity than X-ray.
Although lung ultrasound abnormalities are more common in patients who experience adverse outcomes with COVID-19, few studies have examined whether scans performed early in the hospitalization can provide meaningful risk stratification. Furthermore, few scoring tools predict the need for oxygen on discharge, which represents a limited resource in many settings. In the latest study, the researchers examined whether early pulmonary POCUS findings correlate with important clinical outcomes, such as intensive care admission or need for supplemental oxygen. They also examined whether these findings, if detected early, are predictive of future clinical outcomes in the subsequent hospital course or after discharge.
In this prospective cohort study conducted at four medical centers of patients hospitalized with COVID-19, the researchers found that lung ultrasounds collected within 24 hours of emergency department triage were predictive of important clinical outcomes in the subsequent hospital course, including ICU admission, intubation, supplemental oxygen usage, and the need for oxygen at discharge. Ultrasound findings associated with an adverse clinical course included B-lines and consolidations (particularly in the anterior and lateral lung fields), while a normal ultrasound on triage was protective against adverse outcomes. Notably, ultrasound findings did not dynamically change over a 28-day window after symptom onset, suggesting that the presence of B-lines or consolidations, regardless of when they are detected, may be important clinical predictors.
Previous investigations have demonstrated that lung POCUS findings (such as B-lines or consolidations) are associated with critical illness and intubation for COVID-19. The new study expands on these observations by demonstrating that scans collected within 24 hours of ED triage may predict outcomes for the entire hospital course, including future supplemental oxygen usage and the need for oxygen on discharge. This information may substantially aid frontline providers in resource-limited settings experiencing patient surges. In such scenarios, POCUS could augment admission or discharge decisions for providers. More broadly, POCUS could represent one of several tools to identify patients at-risk for adverse outcomes. Other authors have demonstrated the utility of laboratory tests (eg, ferritin, c-reactive protein) or radiographic findings for risk stratification. POCUS may have potential advantages over these other methods in that it is more expedient, low cost and does not expose the patient to ionizing radiation. Future studies are needed to directly compare POCUS with other scoring systems that utilize laboratory or radiological findings.
Related Links:
Stanford University
Latest COVID-19 News
- Low-Cost System Detects SARS-CoV-2 Virus in Hospital Air Using High-Tech Bubbles
- World's First Inhalable COVID-19 Vaccine Approved in China
- COVID-19 Vaccine Patch Fights SARS-CoV-2 Variants Better than Needles
- Blood Viscosity Testing Can Predict Risk of Death in Hospitalized COVID-19 Patients
- ‘Covid Computer’ Uses AI to Detect COVID-19 from Chest CT Scans
- MRI Lung-Imaging Technique Shows Cause of Long-COVID Symptoms
- Chest CT Scans of COVID-19 Patients Could Help Distinguish Between SARS-CoV-2 Variants
- Specialized MRI Detects Lung Abnormalities in Non-Hospitalized Long COVID Patients
- AI Algorithm Identifies Hospitalized Patients at Highest Risk of Dying From COVID-19
- Sweat Sensor Detects Key Biomarkers That Provide Early Warning of COVID-19 and Flu
- Study Assesses Impact of COVID-19 on Ventilation/Perfusion Scintigraphy
- CT Imaging Study Finds Vaccination Reduces Risk of COVID-19 Associated Pulmonary Embolism
- Third Day in Hospital a ‘Tipping Point’ in Severity of COVID-19 Pneumonia
- Longer Interval Between COVID-19 Vaccines Generates Up to Nine Times as Many Antibodies
- AI Model for Monitoring COVID-19 Predicts Mortality Within First 30 Days of Admission
- AI Predicts COVID Prognosis at Near-Expert Level Based Off CT Scans
Channels
Artificial Intelligence
view channel
AI-Powered Algorithm to Revolutionize Detection of Atrial Fibrillation
Atrial fibrillation (AFib), a condition characterized by an irregular and often rapid heart rate, is linked to increased risks of stroke and heart failure. This is because the irregular heartbeat in AFib... Read more
AI Diagnostic Tool Accurately Detects Valvular Disorders Often Missed by Doctors
Doctors generally use stethoscopes to listen for the characteristic lub-dub sounds made by heart valves opening and closing. They also listen for less prominent sounds that indicate problems with these valves.... Read moreCritical Care
view channel
Powerful AI Risk Assessment Tool Predicts Outcomes in Heart Failure Patients
Heart failure is a serious condition where the heart cannot pump sufficient blood to meet the body's needs, leading to symptoms like fatigue, weakness, and swelling in the legs and feet, and it can ultimately... Read more
Peptide-Based Hydrogels Repair Damaged Organs and Tissues On-The-Spot
Scientists have ingeniously combined biomedical expertise with nature-inspired engineering to develop a jelly-like material that holds significant promise for immediate repairs to a wide variety of damaged... Read more
One-Hour Endoscopic Procedure Could Eliminate Need for Insulin for Type 2 Diabetes
Over 37 million Americans are diagnosed with diabetes, and more than 90% of these cases are Type 2 diabetes. This form of diabetes is most commonly seen in individuals over 45, though an increasing number... Read moreSurgical Techniques
view channel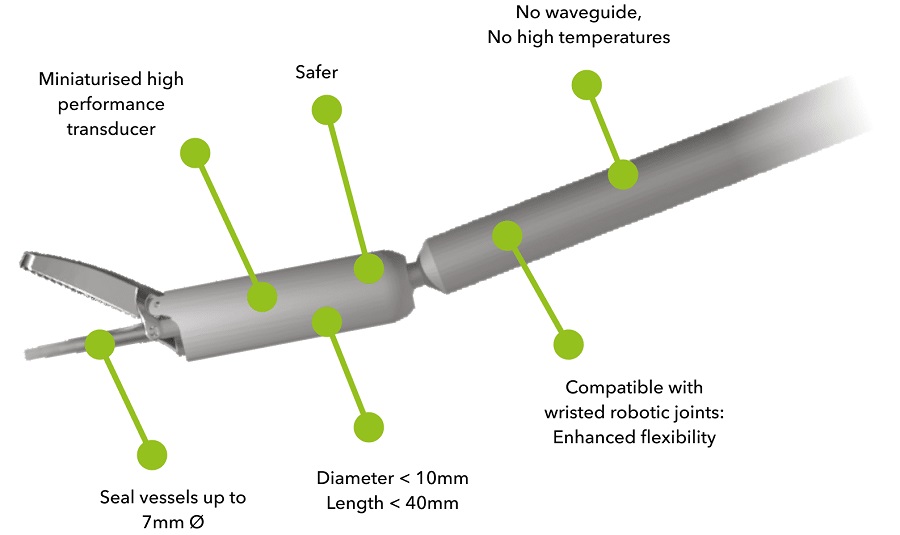
Miniaturized Ultrasonic Scalpel Enables Faster and Safer Robotic-Assisted Surgery
Robot-assisted surgery (RAS) has gained significant popularity in recent years and is now extensively used across various surgical fields such as urology, gynecology, and cardiology. These surgeries, performed... Read moreAI Assisted Reading Tool for Small Bowel Video Capsule Endoscopy Detects More Lesions
A revolutionary artificial intelligence (AI) technology that has proven faster and more accurate in diagnosing small bowel bleeding could transform gastrointestinal medicine. AnX Robotica (Plano, TX,... Read more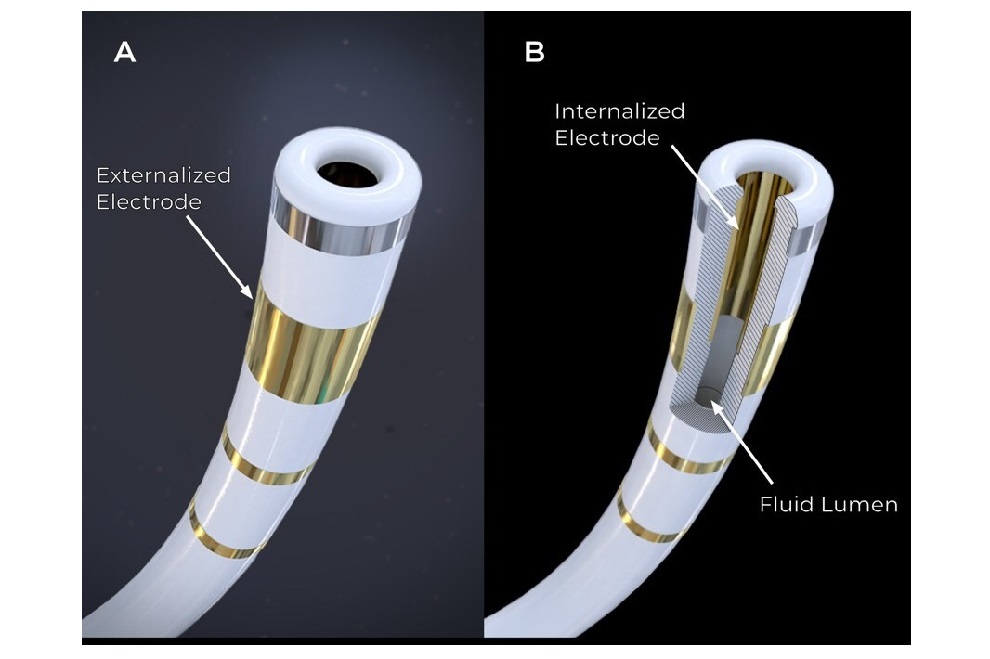
First-Ever Contact Force Pulsed Field Ablation System to Transform Treatment of Ventricular Arrhythmias
It is estimated that over 6 million patients in the US and Europe are affected by ventricular arrhythmias, which include conditions such as ventricular tachycardia (VT) and premature ventricular contractions (PVCs).... Read more
Caterpillar Robot with Built-In Steering System Crawls Easily Through Loops and Bends
Soft robots often face challenges in being guided effectively because adding steering mechanisms typically reduces their flexibility by increasing rigidity. Now, a team of engineers has combined ancient... Read morePatient Care
view channelFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read more
Point of Care HIV Test Enables Early Infection Diagnosis for Infants
Early diagnosis and initiation of treatment are crucial for the survival of infants infected with HIV (human immunodeficiency virus). Without treatment, approximately 50% of infants who acquire HIV during... Read more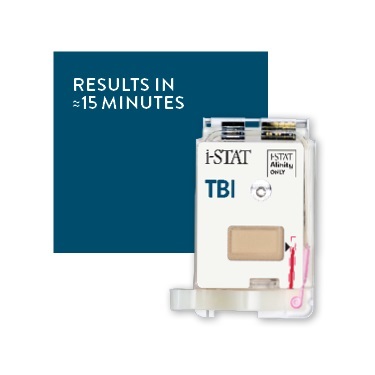
Whole Blood Rapid Test Aids Assessment of Concussion at Patient's Bedside
In the United States annually, approximately five million individuals seek emergency department care for traumatic brain injuries (TBIs), yet over half of those suspecting a concussion may never get it checked.... Read more
New Generation Glucose Hospital Meter System Ensures Accurate, Interference-Free and Safe Use
A new generation glucose hospital meter system now comes with several features that make hospital glucose testing easier and more secure while continuing to offer accuracy, freedom from interference, and... Read moreBusiness
view channel
Johnson & Johnson Acquires Cardiovascular Medical Device Company Shockwave Medical
Johnson & Johnson (New Brunswick, N.J., USA) and Shockwave Medical (Santa Clara, CA, USA) have entered into a definitive agreement under which Johnson & Johnson will acquire all of Shockwave’s... Read more