First-of-Its-Kind Wearable, Non-Invasive and Needle-Free Device Monitors Glucose Levels in Sweat
|
By HospiMedica International staff writers Posted on 18 Oct 2021 |
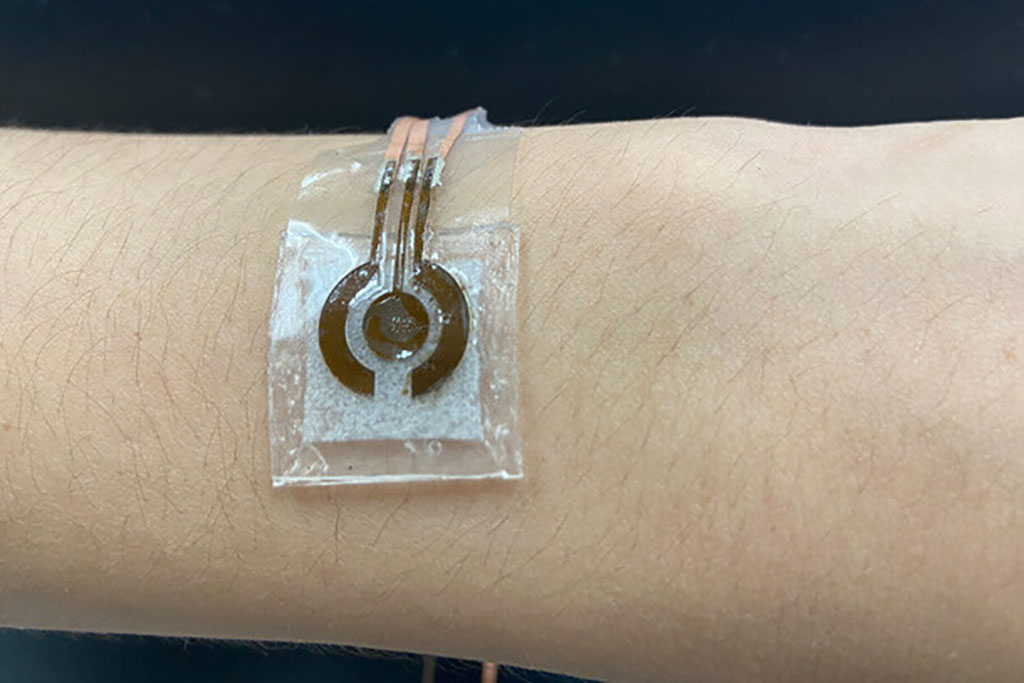
Researchers have developed a prototype of a wearable, non-invasive glucose sensor to be worn on the arm that could make less intrusive glucose monitoring the norm.
The first-of-its-kind wearable, non-invasive low-cost sensor developed by researchers at Penn State (University Park, Pa.) can detect glucose in sweat. Non-invasive glucose monitoring devices are not currently commercially available in the US, so people with diabetes must collect blood samples or use sensors embedded under the skin to measure their blood sugar levels. The researchers constructed the device first with laser-induced graphene (LIG), a material consisting of atom-thick carbon layers in various shapes. With high electrical conductivity and a convenient fabrication time of just seconds, LIG appeared to be an ideal framework for the sensing device - but there was a significant caveat.
The team chose nickel because of its robust glucose sensitivity and combined it with gold to lower potential risks of an allergic reaction. The researchers hypothesized that the LIG outfitted with the nickel-gold alloy would be able to detect low concentrations of glucose in sweat on the skin’s surface. A material with high glucose sensitivity was a priority. Sweat exhibits remarkably low glucose concentrations compared to blood, although there is a strong correlation between glucose levels in sweat and blood. While the concentration of glucose in sweat is about 100 times less than the concentration in blood, the team’s device is sensitive enough to accurately measure the glucose in sweat and reflect the concentration in blood.
The nickel-gold alloy’s sensitivity allowed the team to exclude enzymes, which are often used to measure glucose in more invasive, commercially available devices or in non-invasive monitors proposed by other researchers. These enzymes, however, can degrade quickly with time and changing temperatures. Non-enzymatic sensors require alkaline solution, which can damage the skin and typically limits device wearability. To curb this issue, the researchers attached a microfluidic chamber to the LIG alloy. This chamber is smaller than previously developed configurations to promote wearability and porous to allow for a range of movement, such as stretching or crushing. It is connected to a collection inlet that passes sweat into the solution without allowing the solution to touch the skin. The basic solution interacts with the glucose molecules to produce a compound that reacts with the alloy. This reaction triggers an electrical signal, indicating the concentration of glucose in the sweat.
With a smaller alkaline solution chamber, the entire device is roughly the size of a quarter and is flexible enough to maintain a secure attachment to the human body. In a proof-of-concept test, the researchers used a skin-safe adhesive to attach the reusable device to a person’s arm one hour and three hours after a meal. The subject performed a brief workout - just enough to produce sweat - right before each measurement time. A few minutes after collecting the sweat, the researchers found that the detected glucose concentration dropped from the first measurement to the next. The glucose measurements from the device were verified by measurements made with a commercially available glucose monitor.
The researchers now plan to improve upon their prototype for future applications, including addressing how patients or clinicians may use the sensor for incremental glucose measurements or continuous monitoring to determine treatment actions, such as administering insulin. They also intend to refine and expand this platform for more comfortable monitoring of other biomarkers that can be found in the sweat or interstitial fluids that fill the space between cells in the body.
“We want to work with physicians and other health care providers to see how we can apply this technology for daily monitoring of a patient,” said Huanyu “Larry” Cheng, Dorothy Quiggle Career Development Professor in Penn State's Department of Engineering Science and Mechanics, who led the study. “This glucose sensor serves as a foundational example to show that we can improve the detection of biomarkers in sweat at extremely low concentrations.”
Related Links:
Penn State
Latest Patient Care News
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization

- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- Next Gen ICU Bed to Help Address Complex Critical Care Needs
- Groundbreaking AI-Powered UV-C Disinfection Technology Redefines Infection Control Landscape
- Clean Hospitals Can Reduce Antibiotic Resistance, Save Lives
- Smart Hospital Beds Improve Accuracy of Medical Diagnosis
- New Fast Endoscope Drying System Improves Productivity and Traceability
- World’s First Automated Endoscope Cleaner Fights Antimicrobial Resistance
- Portable High-Capacity Digital Stretcher Scales Provide Precision Weighing for Patients in ER
- Portable Clinical Scale with Remote Indicator Allows for Flexible Patient Weighing Use
- Innovative and Highly Customizable Medical Carts Offer Unlimited Configuration Possibilities
- Biomolecular Wound Healing Film Adheres to Sensitive Tissue and Releases Active Ingredients
- Wearable Health Tech Could Measure Gases Released From Skin to Monitor Metabolic Diseases
- Wearable Cardioverter Defibrillator System Protects Patients at Risk of Sudden Cardiac Arrest
- World's First AI-Ready Infrasound Stethoscope Listens to Bodily Sounds Not Audible to Human Ear
Channels
Artificial Intelligence
view channel
AI-Powered Algorithm to Revolutionize Detection of Atrial Fibrillation
Atrial fibrillation (AFib), a condition characterized by an irregular and often rapid heart rate, is linked to increased risks of stroke and heart failure. This is because the irregular heartbeat in AFib... Read more
AI Diagnostic Tool Accurately Detects Valvular Disorders Often Missed by Doctors
Doctors generally use stethoscopes to listen for the characteristic lub-dub sounds made by heart valves opening and closing. They also listen for less prominent sounds that indicate problems with these valves.... Read moreCritical Care
view channel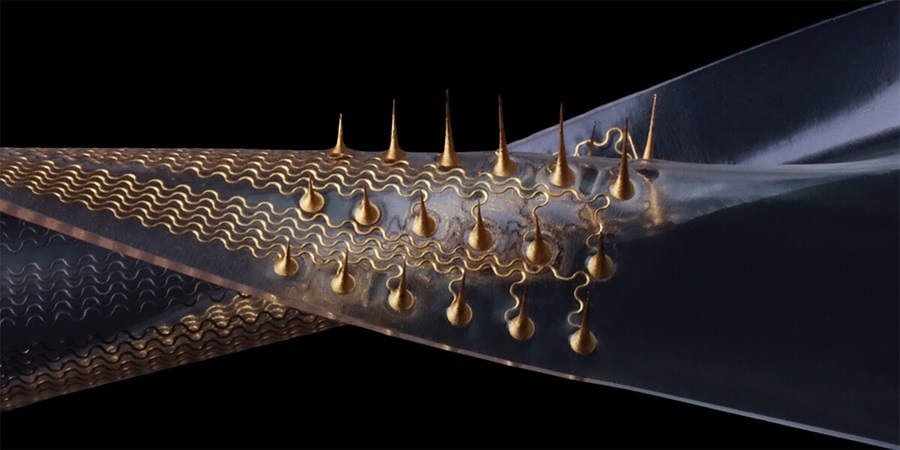
Stretchable Microneedles to Help In Accurate Tracking of Abnormalities and Identifying Rapid Treatment
The field of personalized medicine is transforming rapidly, with advancements like wearable devices and home testing kits making it increasingly easy to monitor a wide range of health metrics, from heart... Read more
Machine Learning Tool Identifies Rare, Undiagnosed Immune Disorders from Patient EHRs
Patients suffering from rare diseases often endure extensive delays in receiving accurate diagnoses and treatments, which can lead to unnecessary tests, worsening health, psychological strain, and significant... Read more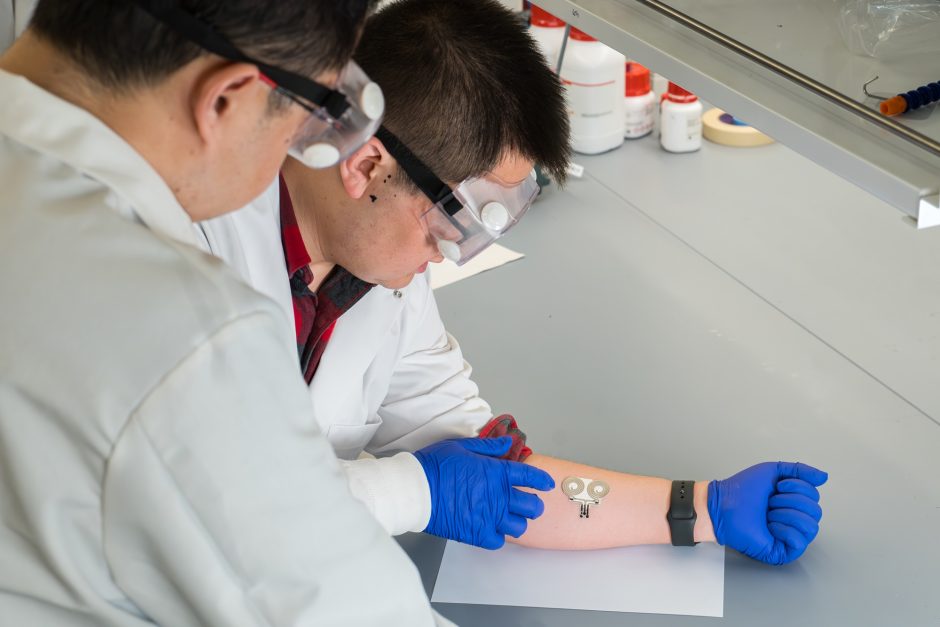
On-Skin Wearable Bioelectronic Device Paves Way for Intelligent Implants
A team of researchers at the University of Missouri (Columbia, MO, USA) has achieved a milestone in developing a state-of-the-art on-skin wearable bioelectronic device. This development comes from a lab... Read more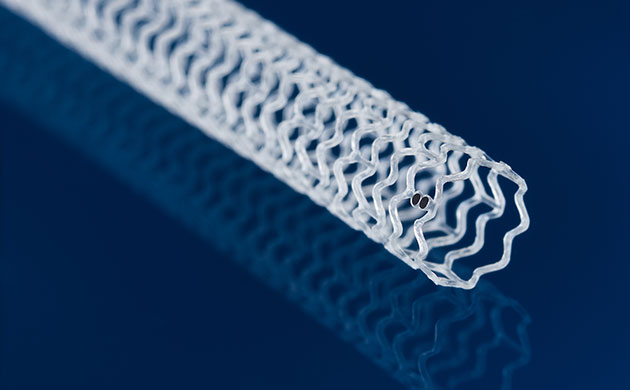
First-Of-Its-Kind Dissolvable Stent to Improve Outcomes for Patients with Severe PAD
Peripheral artery disease (PAD) affects millions and presents serious health risks, particularly its severe form, chronic limb-threatening ischemia (CLTI). CLTI develops when arteries are blocked by plaque,... Read moreSurgical Techniques
view channel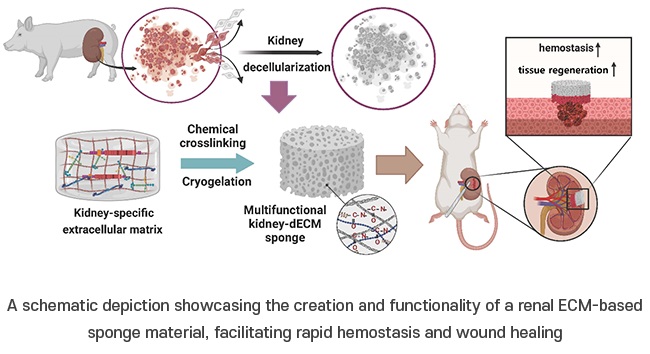
Porous Gel Sponge Facilitates Rapid Hemostasis and Wound Healing
The kidneys are essential organs that handle critical bodily functions, including waste elimination and blood pressure regulation. Often referred to as the silent organ because they typically do not manifest... Read more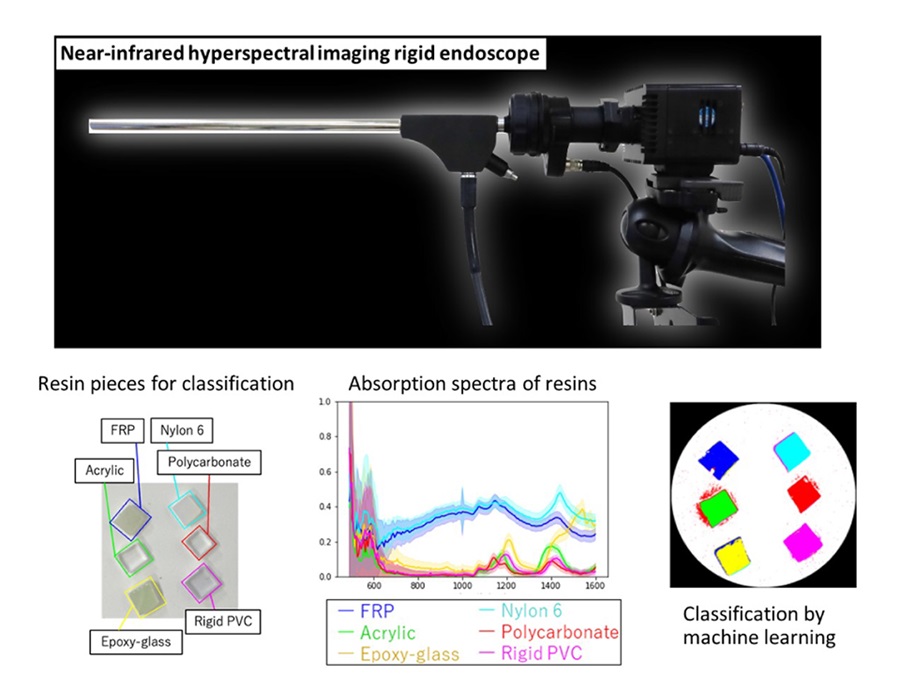
Novel Rigid Endoscope System Enables Deep Tissue Imaging During Surgery
Hyperspectral imaging (HSI) is an advanced technique that captures and processes information across a given electromagnetic spectrum. Near-infrared hyperspectral imaging (NIR-HSI) has particularly gained... Read more
Robotic Nerve ‘Cuffs’ Could Treat Various Neurological Conditions
Electric nerve implants serve dual functions: they can either stimulate or block signals in specific nerves. For example, they may alleviate pain by inhibiting pain signals or restore movement in paralyzed... Read more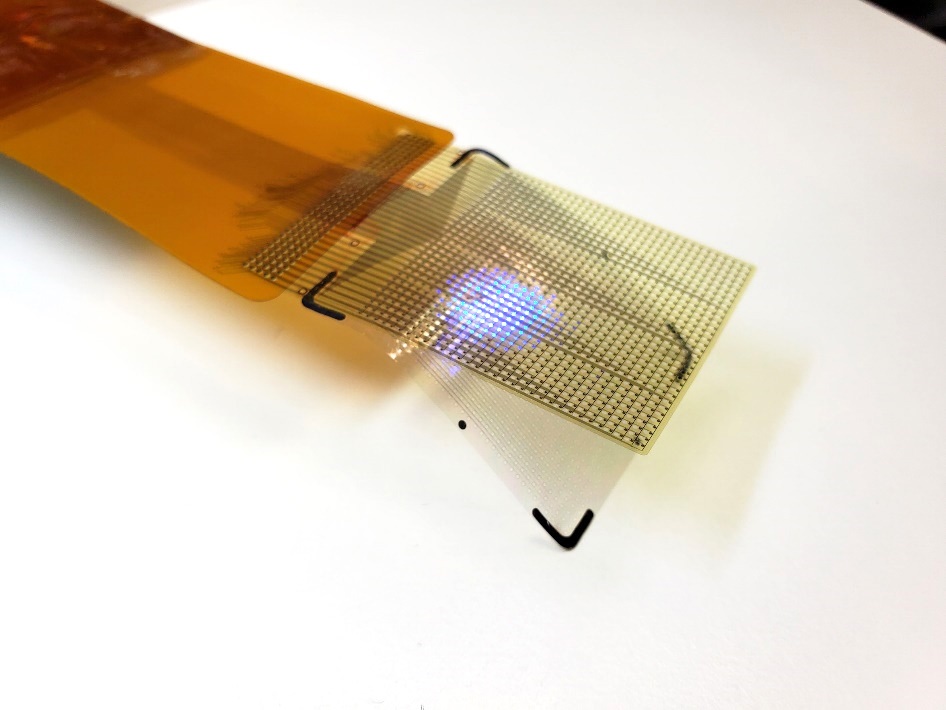
Flexible Microdisplay Visualizes Brain Activity in Real-Time To Guide Neurosurgeons
During brain surgery, neurosurgeons need to identify and preserve regions responsible for critical functions while removing harmful tissue. Traditionally, neurosurgeons rely on a team of electrophysiologists,... Read morePatient Care
view channelFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read more
Point of Care HIV Test Enables Early Infection Diagnosis for Infants
Early diagnosis and initiation of treatment are crucial for the survival of infants infected with HIV (human immunodeficiency virus). Without treatment, approximately 50% of infants who acquire HIV during... Read more
Whole Blood Rapid Test Aids Assessment of Concussion at Patient's Bedside
In the United States annually, approximately five million individuals seek emergency department care for traumatic brain injuries (TBIs), yet over half of those suspecting a concussion may never get it checked.... Read more
New Generation Glucose Hospital Meter System Ensures Accurate, Interference-Free and Safe Use
A new generation glucose hospital meter system now comes with several features that make hospital glucose testing easier and more secure while continuing to offer accuracy, freedom from interference, and... Read moreBusiness
view channel
Johnson & Johnson Acquires Cardiovascular Medical Device Company Shockwave Medical
Johnson & Johnson (New Brunswick, N.J., USA) and Shockwave Medical (Santa Clara, CA, USA) have entered into a definitive agreement under which Johnson & Johnson will acquire all of Shockwave’s... Read more